Introduction↑
Even though the so-called "Spanish" influenza pandemic of 1918-1919 coincided in part with the final year of World War I, and even though it claimed four to five times more lives than did the war, it is not a subject to which historians of that war have given much attention. Indeed, for nearly eighty years they virtually ignored it. Only in the last two decades has it begun to find its way into accounts of 1918, and then largely in passing or only to be dismissed as of little relevance to the war.
Accordingly, it is not historians of World War I who have investigated the relationship of the Great War and the Great Flu, but rather a growing number of social and medical scientists who took advantage of an intellectual terrain increasingly congenial to such inquiry. In the 1970s, for instance, the emergence of environmental history, the social history of medicine, oral history and urban history provided such a facilitating milieu, and to this other factors have since added further incentives to pursue such questions and also enhanced scholars' capacity to do so. These include the turn to global/ world/ transnational history in the discipline, the high-profile re-construction of the causative virus of the 1918-19 pandemic through archaeological virology, repeated outbreaks of avian influenza epidemics around the world since 1997, the brief but frightening appearance of the flu-like SARS (Severe Acute Respiratory Syndrome) epidemic in 2003, and the rising threat of bioterrorism, especially since 9/11. One marker of this growing interest in the 1918-19 pandemic in all its aspects is the publication over the last dozen years of over fifty books and theses and five times as many scholarly articles on the pandemic, while at least five TV documentaries on the subject have been screened.[1]
Drawing on the findings and insights of this recent wave of writing about the pandemic, this article seeks to explore its origins, contemporary perceptions of it, its demographic, administrative and social impact and, finally, how far it and World War I were connected to each other.
The virus and its transmission↑
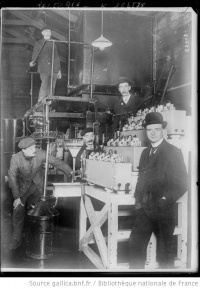
The “Spanish” flu pandemic was, quite simply, the single worst disease episode in modern world history. In the space of eighteen months in 1918-1919, its three waves killed some 50 million people around the globe, or some 3 to 4 percent of the world’s population. To explain this catastrophe, one must first understand the influenza virus and its behaviour. Like all viruses, the influenza virus’ primary aim is to replicate itself. To this end, it long ago adapted its effect on humans so as to maximize its opportunities to spread from person to person. Thus, the characteristic symptoms which it produced – sneezing and coughing – are tailor-made to spread it where people are in close proximity to each other. For example, of the 40,000 droplets which the average influenza-induced sneeze yields, it requires only one containing the influenza virus to infect someone nearby, either through direct transmission into their eyes, nostrils or mouth or indirectly through inhalation from the suspended aerosol.
All of this means that the optimal condition for the spread of the influenza virus is an environment densely packed with human beings, such as military barracks, troopships, troop trains, prisoner-of-war camps, labour compounds, factories, mine-shafts, schools, mass meetings and processions. In other words, influenza is a disease of crowds par excellence, a social phenomenon which World War I consistently created on a large scale.
A possible path to a lethal pandemic↑
These were the congenial circumstances that the most mutable of the influenza viruses, type A, seems to have begun to take advantage of as early as 1915-1916, when hindsight reveals a rise in the incidence of an unusual strain of influenza in countries as far apart as Finland, India, France, Germany and the USA.[2]
Best documented are outbreaks in 1916 and 1917 of what was then dubbed "purulent bronchitis", which occurred in two big military camps, at Étaples in north-western France and at Aldershot in south-eastern England. Despite having this label attached to it, with retrospect the disease’s symptoms seem to resemble those of the later "Spanish" flu, especially the heliotrope cyanosis which the latter produced in serious cases. However, "purulent bronchitis" lacked the ability to spread beyond the two camps and so in April 1917 the causative virus appears to have dipped out of view for the time being, though not out of existence.
Perhaps having undergone further mutation among the millions of troops on the move during the succeeding months – including those from the USA which had entered the war in April 1917 – what was now a re-assorted, more infectious influenza A virus re-appeared in public in March 1918 in rural Kansas, and soon after this at two jam-packed US military camps, the one nearby at Camp Funston, Fort Riley, and the other at Camp Oglethorpe in Georgia. Mass troop movements ensured that the now far more infectious virus spread rapidly from these camps to many other military bases in North America, to the civilian population and then across the Atlantic to Britain and France, primarily aboard troopships. From this heartland of the world war and world trade, it was then spread to several parts of the northern hemisphere by similar means between May and July 1918.
Though this first wave of the pandemic laid millions low, it claimed relatively few lives and was most noted for the disruption of everyday activities which it caused among troops and civilians alike and for the fact that such disruptions in neutral Spain (where no censorship of the press was in force) were widely reported in the world’s media, earning it the mistaken tag of "Spanish" flu. Already on 2 June 1918, the Times’ Madrid correspondent referred to it as "The Spanish Epidemic",[3] while three weeks later that newspaper breezily reported that "Everybody thinks of it as the Spanish influenza today ... The man in the street ... cheerfully anticipated its arrival here [in Britain].”[4] In this light-hearted vein, the English satirical magazine, Punch, announced that "Spain has rendered itself unpleasantly conspicuous by developing and exporting a new form of influenza ....”[5] But the downside of an attack by this flu soon became apparent wherever it struck. In Mumbai, for instance, "Nearly every house ... has some of its inmates down with [influenza] fever and every office is bewailing the absence of clerks,” noted the Times of India late in June,[6] while in Russia Pravda wrote that “Ispanka [the Spanish Lady]” had thrown the town of Murom into disarray.[7] Even the frontline of the battlefield was not unaffected by the pandemic. The joint supreme commander of the German army’s spring 1918 offensive, Erich Ludendorff (1865-1937), complained that, "It was a grievous business having to listen every morning to the Chiefs of Staff’s recital of the number of influenza cases, and their complaints about the weakness of their troops.”[8]
So rapid a passage through millions of respiratory systems during this first wave of the “Spanish” flu pandemic did not leave the virus unaffected either. Going by what happened in the next four months, it would seem that sometime in August 1918, the A virus serotype already circulating so extensively, mutated yet again, this time into an H1N1 subtype which added to its existing high infectivity the ability easily to penetrate deep into the lungs which it then attacked with speed and ferocity.
This viral assault triggered an over-vigorous immune response (a so-called “cytokine storm”) in those with robust immune systems (most commonly young adults), causing viral pneumonia and severe ARDS (adult respiratory distress syndrome), with its telltale bluish discoloration of the skin because of a lack of oxygen (known as “heliotrope cyanosis”), or it laid the way open for bacteria to produce pneumonia on their own. In either case the symptoms were dire – laboured breathing, crackling sounds from the lungs, a racking cough and a pungent odour – and the effects often lethal.
It is surely no coincidence that the newly mutated H1N1 virus which created the deadly second wave of “Spanish” flu first made its transformed presence known late in August 1918 in Freetown, Brest and Boston, three major wartime ports through which hundreds of thousands of soldiers and sailors had been streaming since the first wave of the pandemic had broken out earlier in the year.
In Freetown, Sierra Leone it first appeared on a large scale among the harbour’s colliers and stevedores, and from them it was easily transmitted to sailors, soldiers and passengers aboard ships calling there. In turn, when these shipboard vectors reached their next destination, the infectious among them spread it to locals. By this process of primary and secondary diffusion the second wave of the pandemic quickly reached ports in West and South Africa, and from these their respective hinterlands via rail and road. It was, in sum, a pandemic driven by the steam-engine, whether at sea or on land.
The pattern of diffusion in Europe (from Brest) and the Americas (from Boston) was not dissimilar, with infected soldiers and sailors once again being the principal carriers. Appropriately, therefore, a recent article on the spread of the “Spanish” flu on Newfoundland is entitled “Boats, Trains, and Immunity.”[9] By such means the deadly second wave of the pandemic circled the globe in the last quarter of 1918, leaving no continent and but a handful of isolated islands untouched by its heavy hand.
Soldiers and sailors, whether on-duty or on leave, AWOL or taken prisoner, demobilized or repatriated, were supplemented as efficient flu vectors by migrant labourers, refugees, pilgrims, school pupils and large gatherings of people at places of work, worship and procession. In other words, everyday activities became fraught with the danger of infection. As one flu survivor recalled, a sneeze or a cough became a terrifying sound to all in its immediate vicinity.[10]
The fact that over half of the world’s population had been infected by this runaway H1N1 virus meant that those who survived probably gained a broad immunity to it, at least temporarily. Thus, when, in the first half of 1919, the virus re-surfaced in a slightly altered form as a third global wave of “Spanish” flu, against the background of the movement of post-war refugees, soldiers being repatriated and peacetime commerce resuming, its capacity to infect and kill was diminished. Even so, it claimed some 2 to 3 million lives worldwide in those six months. Yet, relative to the second wave’s ravages, this was a small number which made the third wave appear quite moderate to relieved contemporaries who had been expecting the worst.
The differentiated demographic impact↑
Even if the figures are only estimates, in terms of lives claimed, World War I (ca. 12-14 million dead) is dwarfed by the three waves of the “Spanish” influenza pandemic which killed, directly or indirectly, ca. 50 million people. Of course, only the pandemic of influenza was truly global in its compass – the so-called “world” war involved fewer than two-thirds of the fifty-six states and empires then in existence.
Among these fifty-six, the flu death-toll varied greatly, from 23.6 percent of the small population of Western Samoa to 0.14 percent of all Uruguayans.[11] In general, the islands of the Pacific, sub-Saharan Africa, South and East Asia and Central America were hit worst: Europe and North America least so. Yet, even within a single country, considerable differences in mortality occurred. For example, in the adjoining rural districts of Mount Frere and Mount Ayliff in South Africa, the mortality rates were 7.8 percent and 1.4 percent respectively,[12] while in the USA Philadelphia lost nearly 1 percent of its population but Baltimore just 0.83 percent, although the two cities were only 100 miles apart.[13] Most striking of all was the disparity in “Spanish” influenza mortality between Western Samoa (8,500 deaths) and American Samoa (0 deaths) just 40 miles away.[14]
Several factors help to explain these marked differences in mortality. In the case of the two Samoas, a very strict quarantine had been imposed on American Samoa by its governor, which effectively excluded the virus from the island, unlike on Western Samoa where an open-port status was maintained by its New Zealand administration.
What most distinguished Philadelphia from Baltimore in 1918 was that, in the former, patriotic Liberty Loan Drive parades continued all through the duration of the epidemic there, drawing thousands together in its streets. One such parade, on 28 September 1918, attracted 200,000 participants; three days later, 635 new cases of “Spanish” flu were reported. In Baltimore, such mass gatherings were prohibited, though not without considerable opposition from the city’s Health Commissioner first.
Finally, the telling difference between the Mount Frere and the Mount Ayliff districts is that the latter had been exposed to the first wave of the pandemic, but not the former. Consequently, while many in Mount Ayliff contracted first-wave “Spanish” influenza, few died of it. Thus, when the lethal second-wave arrived soon afterwards, many had a degree of immunity to it. Such preventive prior exposure was not vouchsafed to their neighbours in Mount Frere when the second wave hit them.
Differing circumstances such as in the three cases outlined above go a long way towards accounting for otherwise puzzling contrasts in pandemic mortality, between countries like Australia and New Zealand (here the first imposed a strict quarantine but not the second), between mining towns like Johannesburg and Kimberley (here the former was exposed to the first wave but not the latter, before both were hit by the second wave) and even between two suburbs of the same city, like Kensington and Southwark in London (where their strikingly different class composition translated into living and working environments less or more congenial to the transmission of the influenza virus and to the availability or non-availability of nurses to tend flu victims). Indeed, given the importance of proximity to an infected person in facilitating the spread of the virus, the degree of overcrowding and contact with others should be an integral part of every attempted explanation of its diffusion. This may help to explain why people in occupations in which encounters with the public were common, like bus and train conductors, shopkeepers, shop assistants and bank and postal clerks, were especially vulnerable to infection, as some analyses suggest.[15]
If the geographic and occupational variability of the pandemic’s impact was primarily a function of time, space, class and edict, the age-structure of those whom it killed derived principally from physiology and age-, gender- and society-related modes of behaviour. To understand this, it is necessary to differentiate between the 500+ million who contracted the disease – as far as it is possible to tell, this figure encompassed all ages, classes and both sexes – and some 50 million who then died of it. The latter were disproportionately those aged between eighteen and forty, and more often male than female, save if the women were pregnant. This, it should be noted, is a pattern entirely at odds with the usual profile of those killed by influenza, i.e. those whose immune systems are still developing (the young) or have begun to weaken (the old).
Explaining this anomaly requires awareness not only of the existence of the “cytokine storm” effect in those with the most robust immune systems (see above), but also of the contemporary concept of masculinity in which “real” men did not stay in bed if they had as common an ailment as a dose of flu, but soldiered on in the trenches or, if breadwinners, got up and went to work to support their families. Given that the only really effective treatment for “Spanish” influenza in 1918 was bedrest and good nursing so as to minimize physical stress and maximize supportive care, a “get-up-and-go” attitude was extremely dangerous to life. The 1916 edition of Black’s Medical Dictionary recognized exactly this danger, noting that, in a case of influenza, “the person must perforce take to bed, but it is not at all uncommon for vigorous people to struggle on with their usual work. This is very unwise ...”[16]
Indeed, it is likely that the absence of skilled nursing in the home – whether because of class, cultural barriers or sheer unavailability as a result of the wartime demand for nurses – may have been a significant factor in determining case mortality. If the poor, those unable to get into jam-packed hospitals and those in remote areas died in disproportionate numbers – as some have argued[17] – then this may be the chief reason why.
Although it is natural to focus on the staggering number who died in the pandemic – perhaps 10 percent of all who contracted it or 3-4 percent of the entire world population at the time – it is as important to notice too its further, long-term demographic effects. In view of the high number of pregnant women who died in the pandemic because of their enhanced vulnerability to respiratory and cardiovascular stress – “those most likely of the most likely to die,” one historian has labelled them[18] – the unknown number of babies not born as a result of their would-be mother’s death must be included in the toll too. In addition, to these should be added babies miscarried, aborted or stillborn as a result of their mothers having contracted “Spanish” flu. In seventeen American states, for example, stillbirths rose by 60 percent in October 1918.[19] Moreover, should the number of babies never conceived because of the death of their yet-to-become mothers not be considered part of the ultimate toll too, at least in the big demographic picture? Certainly the results of these lost and averted births in 1918 or 1919 were to be seen in countries devastated by the pandemic, where school authorities noticed a decline in the number of new school entrants in 1925. As a puzzled Superintendent-General of Education in the Cape Province of South Africa put it, there had been a “slackening in growth” in school enrolment. The missing children were, of course, those who should have been born in 1919 but were not because of their mothers’ “Spanish influenza.”[20]
Nor did the pandemic’s long-term demographic impact end there. The fact that those with pre-existing respiratory diseases were more likely than those without to succumb to the pandemic “culled” many of the former from the population prematurely. One unexpected result was that in the USA, at least, tuberculosis deaths actually fell after 1918 because the pool of those with this disease had been reduced by the influenza pandemic, making the latter an unlikely factor in the decline of tuberculosis in that country. The pandemic also cast a long shadow health-wise. An unknown percentage of those who survived a severe bout of “Spanish” flu were left with their lungs or other organs permanently impaired. Susceptibility to other diseases like nephritis, meningitis, encephalitis lethargica and Parkinson’s disease was attributed by many doctors in the 1920s to an attack of "Spanish" flu in 1918 or 1919.
Even longer-lasting may have been the effect on foetuses in the wombs of mothers who contracted “Spanish” flu but did not die of it. A recent analysis of census data from 1960-1980 revealing that the social profile of Americans born between January and September 1919 (i.e. babies that had been in utero at the height of the pandemic) points to their being marked underachievers compared to cohorts born just before or just after them. In terms of levels of education and income, they were noticeably less successful than their near-contemporaries and far more likely to be disabled or to be recipients of welfare grants.[21] Was this the result of foetal distress caused by their mothers having suffered a bout of “Spanish” flu during the second or third wave of the pandemic? If so, it would extend the direct physical effects of the pandemic by sixty to seventy years.
Equally long-lasting, but in emotional and psychological terms, was the grief caused by the sudden mass death which stemmed from the pandemic. Families shattered by the death of a young parent or spouse and orphans created by the hundred million all bore testimony to the trauma flowing from these deaths, in many cases for the rest of their lives. In 1998 a ninety-year-old South African flu orphan told me that his mother had died in the 1918 pandemic when he was ten, “and I have missed her ever since.”[22] In the same year a second nonagenarian recalled poignantly that when his mother had died of “Spanish” flu in Illinois in 1918, the shine went out of everything ... I realized, for the first time and forever, that we were not safe. We were not beyond harm. My father did what he could. He kept us together as a family, but from that time on there was a sadness which had not existed before, a deep down sadness that never went away.[23]
But back in 1919, most flu widows who had lost their breadwinner husbands had little time to dwell on their loss, being forced to find immediate ways to support their children. Turning to their families for assistance, moving into cheaper accommodation or entering the job market must have been a commonplace experience globally for women in this situation. “My dear husband died of flu, leaving me with five children in poverty and debt,” admitted one such flu widow in rural South Africa. “Pray for me for acceptance and strength. I plan to go to the diamond diggings to see if I can make a living. I will give a tithe to the Lord. Ask the Lord for relief and help.”[24] Many a micro-history will be needed before historians can accurately map such trends and their variations world-wide.
Perceptions and explanations↑
Even some children born during the pandemic’s height, whose parents did not fall victim to it, bore its mark for the rest of their lives by virtue of their names. Baptizing newborns “Ora Pro Nobis” (“pray for us” in Latin) or “Myra” (“lament” in Hebrew) bore testimony to the fear and grief which the pandemic evoked, while bestowing names like “Fraser” (from “freza,” the flu in Shona, spoken in what was then Southern Rhodesia), “Ogbo Ifelunza” (“influenza age group,” the name given to the age-set born between 1919 and 1921 in Igboland in Nigeria) and “Mesiawa” (“I have survived,” the label given to the Kipsigi age-set born at the same time in south-western Kenya) tell of how deeply the episode impressed itself on locals’ consciousness.[25]
Popular sobriquets given to the disease itself sharply reflect contemporary perceptions of it, that, like all attributions of epidemics in history, it had arisen somewhere else. Thus, in many countries, people readily accepted the label “Spanish” as a descriptor, not only because Spain was where the press said it had begun, but also because it was somewhere else. In turn, indignant Spaniards called it “The Naples Soldier,” after a catchy song in an operetta by that name then being performed in Madrid,[26] or they claimed that it came from the battlefields of France. Not surprisingly, given the extraordinary context of World War I, other popular labels make clear that many people were convinced that it must somehow have been connected with the war. Thus, in Entente countries, tags coined included “war plague,” “Flanders grippe,” “Hun flu,” “Turco-Germanic bacterial criminal enterprise” and “German plague,” as many believed that the war-epidemic link lay in the unburied corpses on the battlefields or the dastardly use of poison gas. “So many were killed in the great war of the white people”, explained indigenous healers in faraway Southern Rhodesia, “that the blood of the dead caused this great sickness,”[27] while in the memory of one elderly flu survivor sixty years later, the war “poisoned the air ... all the bombs and things ... travelled with the wind [around the world].”[28]
Other contemporary names recall fingers pointed at political rather than military foes as the malevolent source of the pandemic – for example, “Bolshevik disease” (a term used by Poles), “Kirghiz disease” (a term used by Russians), "white man’s sickness" (a term used by black South Africans) and “kaffersiekte” or “black man’s disease” (a term used by white South Africans). With swiftness and clarity the direct threat to life posed by the influenza pandemic brought to the surface every underlying prejudice and suspicion about or hostility to “the other.”
As widespread was the idea that the pandemic was a punishment for sin meted out by a supreme divine being, that it was an instrument of what Muslims called the “Takdier [Will] of Allah” or what Dutch Christians termed a “Godsbezoeking” (a divine visitation) or what Irish Catholics believed was “the Will of God.” To Christians the nature of the sin varied greatly, depending on what each denomination felt was gravely wrong in the world: immorality, neglect of religious practice, unbelief, social and sanitary neglect and, of course, the war. “Isn’t it so that the Omniscient mocks all murderous instruments thought out by a sinful science?” asked a Dutch Reformed Church minister in South Africa rhetorically. “Humanity has slain its thousands, but God his ten thousands.”[29]
Indeed, some Christians concluded that the coincidence of the devastating pandemic and the climax of the terrible world war was more than just chance and interpreted this as a sign that deeper things were afoot. It thus is no surprise that in 1918-1921, amidst this physical, emotional and spiritual travail, several charismatic prophets rose up in sub-Saharan Africa, preaching millenarianism, faith healing and the need for instant repentance and renewal. As a result, in Nigeria, the Belgian Congo, Southern Rhodesia and South Africa, inter alia, a number of independent “Aladura” (praying) churches were founded in these years to take forward the visions of these prophets. In triggering their creation, the “Spanish” flu pandemic thus contributed to the emergence of indigenous African Christian sects.
However, within indigenous African religions which saw evil as emanating not so much from a supreme divine being but primarily from ill-intentioned individuals who might even be witches or wizards, the extraordinary mortality caused by the “Spanish” flu produced a spate of “smelling out” by traditional witch-finders, and the resultant punishment of those whom they identified as being behind the evil. “Many cases of homicide and serious assault resulting from ‘smelling out’ have come to my notice recently especially after the outbreak of influenza in the native territories,” reported the Solicitor-General of the Eastern Cape, South Africa in 1919.[30] One consequence of this was the amendment of the local penal code so as to stiffen penalties for those convicted of “witch-finding.”
To no small degree, therefore, the many-sided ways in which the world’s population responded to the pandemic in non-material ways, conceptually, religiously and psychologically, suggest that its members entered the 1920s deeply traumatized, not only by the Great War but also by the Great Flu. Yet, few at the time recognized or acknowledged this and many were left to suffer in silence, “their suffering likely deepened by that very silence,” as one historian of the pandemic in the USA has observed.[31] In Britain, argues another, “The political force of emotions ... particularly those associated with loss and mourning, leading to post-traumatic stress disorder – must be appreciated if we are truly to grasp the political history of Great Britain in the first decade of the interwar period.”[32] Might the same be said of other war-and flu-ravaged countries too?
Medical and public policy consequences↑
For the healing profession worldwide and the governments of all hard-hit countries the pandemic was a comprehensive rout, for neither was able to fulfil its primary function, viz. to safeguard the health of the population in the face of a dire threat. Poignantly, the son of one Cape Town doctor recalled his father’s inability to save the lives of a newly married couple who had contracted “Spanish” influenza. “It was then I first saw my father cry,” he wrote. “He was sobbing in sorrow and in frustration at his impotence.”[33]
Accordingly, as soon as the pandemic had passed, both doctors and politicians sought to do whatever they could to prevent another such catastrophe should the “Spanish” influenza recur, as many experts predicted it would. Official commissions of inquiry were appointed by several countries to investigate exactly what had happened during the pandemic’s runaway course and what should be done to check this should it return, while over 200 in-house specialist reports were commissioned by governments, municipalities and armies around the globe with the same object in mind. In tandem with these, doctors’ reports on their experiences and findings in the pandemic poured forth in medical journals on five continents in a bid to understand the aetiology and nature of what many labelled “epidemic influenza” and to establish whether any particular antidotes or treatment had been effective.
Within laboratories as far apart as London, Paris, Berlin, Boston, Melbourne, Rome, Tokyo, Buenos Aires, Johannesburg and Teheran, a number of medical scientists even attempted to identify the causative pathogen of influenza and how it was transmitted. Since the existing wisdom, that the disease was caused by a bacterium, Pfeiffer’s bacillus, had been shown by the “Spanish” flu experience to be false, they were forced to return to the drawing board with their faith in bacteriology severely shaken and to begin painstaking, step-by-step observation and experimentation from scratch. Not until 1933 was a team at the National Institute of Medical Research in London able to demonstrate conclusively that human influenza was caused by a virus transmitted from person-to-person by coughing or sneezing.
Public policy initiatives to try and prevent a repeat of the disaster of 1918-1919 focused mainly on attempting to create more effective public health systems, either by setting up central public health departments, as in South Africa, Canada, Australia and Great Britain, or by expanding the ambit and capacity of existing governmental public health structures, as in New Zealand, France, India and Mexico. Not surprisingly, all of these countries were among those which readily signed up as members of the international networks which were created in the 1920s by the Office International d’Hygiène Publique in Paris and the League of Nations’ new Health Organization to share information on local epidemic outbreaks. Soon this data was being regularly circulated in monthly bulletins sent out by post.
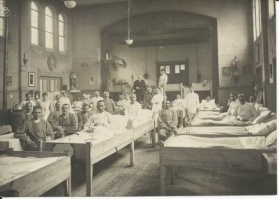
In tandem with these international public health initiatives went the speedy local provision of new hospitals, or at least the expansion of existing ones which the pandemic had shown to be inadequate and outmoded. Either as a catalyst for such construction or as the accelerator of long-stalled plans to accomplish this, the “Spanish” influenza pandemic was of significant influence.
The Great Flu and the Great War↑
As already indicated, many contemporaries firmly believed that the war and the pandemic were connected in some terrible way, either by design or by accident. For millions of super-patriotic English-speakers around the world, the similarity of the words “germs” and “Germans” was all the proof they needed. But a century later such facile associations need to be interrogated critically, especially as few historians of World War I have accepted them. Probing whether such a relationship existed requires recognition of its potentially two-way character, viz. of the effect of the war on the pandemic and vice versa.
At present, no virologist can demonstrate that the ancestor of the causative H1N1 virus was the product of wartime conditions, though recent viral archaeology and reconstruction have suggested that it emerged between 1915 and 1917, i.e. during World War I. Nor is it yet possible to prove that the war was responsible for the re-assortment of the virus into the highly infectious but mild H1N1 virus which drove the first wave of the pandemic or of its subsequent mutation into the lethal virus behind the second wave, although the world context in which these metamorphoses occurred is also suggestive and circumstantial. This context was, of course, World War I, with its mass agglomeration of soldiers in jam-packed barracks, troopships, troop trains and trenches across Europe, Africa, Asia, North America and the Middle East, all tailor-made locations for extensive viral re-assortment to take place. In this situation, the three major wartime ports where the second wave made its public debut, Freetown, Boston and Brest, can justly be perceived as pathogenic entrepôts.
What is clear, however, is that once the H1N1 virus had emerged in these two forms in 1918, its global dispersion owed a great deal to the movement of soldiers and sailors to and from battle-zones by land and sea. Whether it was aboard ships like the Leviathan (Boston to Brest, May 1918), the Khiva (Liverpool to New York, July 1918), HMS Mantua (Plymouth to Freetown, August 1918), the Jaroslav and the Veronej (Freetown to Cape Town, September 1918), the USS Logan (Manila to Guam, October 1918), the Niagra (Honolulu to Auckland, October 1918), the Talune (Auckland to Fiji, Tonga and Western Samoa, November 1918), the Ceramic (London to Albany, Western Australia, March 1919) or the Madonna (Marseilles to Reunion, March 1919) or the trains which met those who disembarked and carried them inland, all were highly efficient vehicles for spreading vectors harbouring the H1N1 virus across oceans and continents. In effect, the H1N1 virus was globalized by World War I which systematically turned a local outbreak in one continent into a world pandemic. In the words of two medical geographers examining the spread of the pandemic to the south Pacific, this was the way in which “a disease agent, first appearing among the military on one side of the world, [was able to] spark a civilian epidemic some 12,000 miles away.”[34]
The war’s insatiable demand for human resources affected the pandemic in other ways too, especially in the treatment of those stricken by it. By 1918 the armies and navies of belligerent countries had drained civilian life of a large percentage of doctors and nurses, leaving citizens at home hard-pressed to secure adequate professional treatment. As a result, some who may have survived a bout of “Spanish” flu if they had received proper medical or nursing care, did not.
On the other hand, the fact that the governments of nations-at-war could deploy uniformed doctors and nurses as they decided meant that, in some countries, such medical personnel could be steered to places in dire need of assistance. Thus, in South Africa, the army’s Deputy-Director of Medical Services (no less) was sent to Kimberley with 100 soldiers to try and turn around the appalling health crisis there, while in the rural Transkei, three army field ambulances, each under a military doctor, toured the flu-stricken region providing medicine and treatment. In New Zealand the Defence Department even furnished emergency civilian hospitals with army beds and with some of the Voluntary Aid Detachment nurses under its charge. “The great value of all of our splendid wartime organisations has become most apparent under the severe tests imposed upon them by this swooping down of the influenza fiend,” commented a Wellington newspaper. “Otherwise it would have been impossible to organise such large numbers of women in such a short space of time.”[35]
The other element in the Great Flu-Great War relationship is the effect of the former on the latter, particularly on its outcome. As even the incomplete estimates in Table 1 reveal, the two waves of the pandemic laid low thousands upon thousands of soldiers on both sides on the Western Front where the outcome of World War I was ultimately decided during 1918. What the table also makes clear is that their prostration was not uniform in either time or scale. Moreover, it is essential to remember that those who contracted but did not die of the “Spanish” flu were hors de combat for weeks rather than days, especially if they had been struck by the second wave. Protracted lassitude and a debilitating lack of vigour were common long after an attack, which made a return to combat readiness a slow affair. “[W]e were leaden-footed for weeks [afterwards]”, recalled one victim, “to the point where each step meant a determined effort.”[36]
| April | May | June | July | August | September | October | |
| German | 77,000 (3.5%) | 135,002 (6.1%) | 374,524 (17.02%) | 420,000 | |||
| French | 24,886 (0.95%) | 12,304 (0.45%) | 2,369 (0.11%) | 3,135 (0.13%) | 24,282 (0.92%) | 75,519 (2.85%) | |
| American | 1,850 | 1,124 | 5,700 | 5,788 | 37,935 | 38,655 (1.9%) | |
| British/Imperial | 36,473 (May and June) | [see May] | 22,136 (1.1%) |
Table 1: Estimated number and/or percentage of reported influenza cases among troops of main combatants on Western Front, April-October 1918[37]
In the light of this, it is necessary to add “Spanish” flu morbidity (as well as mortality) to the trio of manpower-depleting factors primarily responsible for the inability of the German army to achieve success in its five do-or-die offensives on the Western Front between March and July 1918, for its soldiers were struck down by the flu at crucial points during these offensives, preventing them from executing fully their generals’ grand plans for victory. Moreover, as Table 1 shows, their foes were not as disabled by the pandemic at the same time, for it usually arrived in the German lines after it had swept through the ranks of their enemies. For instance, a French officer noted early in July, “In France, it [influenza] is benign ... [b]ut across the front, the Germans are very affected ... [and it is] raging in Germany with intensity.”[38] The influenza virus’ impact was thus not even-handed and so put the German army at a disadvantage against the Allied forces at key moments of decisive battles on the Western Front. That virus should therefore stand alongside bullets, shells, wounds, desertion and capture as the source of Germany’s loss of capacity to drive home the offensives it pursued in its desperate, victory now-or-never campaign.
As early as June 1918 Ludendorff was complaining that the spirit of his troops was “already weakened by influenza,”[39] a situation which caused one general to request a delay in launching the fifth offensive on account of a lack of manpower. Reduced battalion strength “due to the still rampant so-called Spanish influenza” made “a use of force seem questionable,” argued one senior German officer,[40] a circumstance which alert British intelligence officers were quick to pick up as they reported that the large number of German troops down with influenza was “one of the factors which caused the postponement of a certain contemplated attack of very critical importance.”[41] Even with battalion strengths reduced by 25 percent or more, Ludendorff was in denial –“The troops need to get used to weak battle strengths; and I do not know influenza,” he insisted[42] – and the offensive against the French positions eventually went ahead five days late, on 15 July. Three days later, having weathered the compromised German attack as the delay had given them enough time to clear their lines, the French forces began a counter-offensive which gained momentum week-by-week, as more and more American troops joined the fray, gradually forcing the Germans onto the back foot. On 3 August Rupprecht, Crown Prince of Bavaria (1869-1955) wearily noted, “Poor provisions, heavy losses and the deepening influenza have deeply depressed the spirits of the men in the III Infantry Division.”[43] It is a mark of how significant Ludendorff subsequently judged the loss of his men to the “Spanish” influenza to have been in impairing his offensives that, when, late in September, the writing was on the wall for Germany and he himself on the point of a nervous breakdown, he told the army’s Surgeon-General that the recent fresh outbreak of the pandemic in the French army might yet offer Germany a “last chance” against outright defeat, just as in 1762 the sudden “miraculous” death of Elizabeth, Empress of Russia (1709-1762) had saved Prussia from defeat in the Seven Years’ War.[44]
Conclusion↑
Accordingly, to account for the astonishing turnabout on the Western Front between March and September 1918, when Germany went from apparently imminent victory in the wake of the Treaty of Brest-Litovsk to retreat and then defeat, the “Spanish” flu pandemic must be factored into a complex equation already consisting of German corpses, casualties and captives, swelling Allied manpower and materiel and a misconceived and wasteful German military strategy. The stream of events which took Germany, Europe and the world from Brest-Litovsk to Versailles might therefore be conceived of as having been abundantly fed by a Spanish-named tributary as it rolled across the Western Front.
In sum, the Great War and the Great Flu were integral to each other in a host of interacting ways. The inclusion of an article on the latter in a site devoted to the former is thus entirely appropriate, justified and necessary – as would the case be if the situations were reversed.
Howard Phillips, University of Cape Town
Section Editor: Robert Gerwarth
Notes
- ↑ For a selection of these and the earlier works, see the Selected Bibliography. The five professionally made documentaries of which I know are: Influenza 1918 (PBS, The American Experience series, 1998); Pandemic (BBC, Horizon series, 1999); In Search of Spanish Flu (BBC, 2008); Killer Flu (RTE/Radio and Television Ireland, Outbreak series, 2009); We Heard the Bells: The Influenza of 1918 (United States Department of Health and Human Services, 2010) and Die Spanische Grippe - Das große Sterben (2012) [originally released as La grande épidémie (Arte France, 2005)].
- ↑ Johnson, Niall: Britain and the 1918-19 Influenza Pandemic. A Dark Epilogue, Abingdon 2006, pp. 43-5; Erkoreka, Anton: Origins of the Spanish Influenza Pandemic (1918-1920) and Its Relation to the First World War, in: Journal of Molecular and Genetic Medicine, 3,2 (2009), pp. 191-192; Lahaie, Olivier: L'épidémie de grippe dite “espagnole” et sa perception par l'armée française (1918-1919), in: Revue historique des armées, 262 (2011), pp.105-6.
- ↑ The Times, 3 June 1918.
- ↑ The Times, 25 June 1918.
- ↑ Mr. Punch’s History of the Great War. London et al. 1919, p. 241.
- ↑ Quoted in Ramanna, Mridula: Coping with the Influenza Pandemic. The Bombay Experience: in Phillips, Howard and Killingray, David (eds): The Spanish Influenza Pandemic of 1918-19. New Perspectives, London et al. 2003, p. 87.
- ↑ Collier, Richard: The Plague of the Spanish Lady. The Influenza Pandemic of 1918-1919, London et al. 1974, p. 11.
- ↑ Ludendorff, Erich: Ludendorff’s Own Story, August 1914-November 1918, Freeport 1971 reprint of 1920 edition, p. 277.
- ↑ Palmer, C. T., Sattenspiel, L. and Cassidy, C.: Boats, Trains and Immunity: The Spread of the Spanish Flu on the Island of Newfoundland, in: Newfoundland and Labrador Studies, 22, 2 (2007).
- ↑ Anonymous flu survivor in conversation with the author, Kimberley, 18 December 1980.
- ↑ Johnson, Niall and Mueller, Juergen: Updating the Accounts: Global Mortality of the 1918-1920 “Spanish” Influenza Pandemic: in Bulletin of the History of Medicine, 76, 1 (2002), pp. 110-114.
- ↑ Phillips, Howard: Black October: The Impact of the Spanish Influenza Epidemic of 1918 on South Africa, Pretoria 1990, p. 163.
- ↑ Crosby, Alfred: Epidemic and Peace, 1918. Westport et al. 1976, pp. 60-1.
- ↑ Crosby: Epidemic and Peace, pp. 235, 239.
- ↑ McCracken, Kevin and Curson, Peter: Flu Downunder: A Demographic and Geographic Analysis of the 1919 Epidemic in Sydney, Australia in: Phillips and Killingray (eds): Spanish Influenza Pandemic, pp. 124-125.
- ↑ Comrie, John D. (ed.): Black’s Medical Dictionary, 5th edition. London 1916, p. 397C.
- ↑ Bristow, Nancy K.: American Pandemic. The Lost Worlds of the 1918 Influenza Epidemic, Oxford 2012, pp. 131-133.
- ↑ Barry, John M.: The Great Influenza. The Epic Story of the Deadliest Plague in History, New York 2004, p. 239.
- ↑ D. Almond: Is the 1918 Influenza Pandemic Over? Long-Term Effects of In Utero Exposure in the Post-1940 U.S. Population in: Journal of Political Economy, 114, 4 (2006), Figure A1.
- ↑ Cited in Phillips: Black October, p. 125.
- ↑ Almond: Is the 1918 Influenza Pandemic Over?, passim. Following Almond’s lead, other studies have discovered similar characteristics in the life-paths of the Italian, Taiwanese and Brazilian birth-cohorts of 1919 (see Percoco, M.: Spanish Flu and Human Capital Accumulation in Italian Regions, unpublished seminar paper, December 2011, available at: http://didattica.uniboconi.it/mypage/upload/49430_20111212_043611_PERCOCCO_INFLUENZA.PDF; Lin, M-J. and Lin E. M.: Does in Utero Exposure to Illness Matter? The 1918 Influenza Epidemic in Taiwan as a Natural Experiment, available at: http://i.pacdev.ucdavis.edu/files/conference –schedule/sessions/papers/for_MIEDC.pdf; Nelson, R. E.: Testing the Fetal Origins Hypothesis in a Developing Country – Evidence from the 1918 Influenza Pandemic, unpublished paper, May 2008, available at: home.utah.edu/~uo154844/BrazilFluPaper-080827.pdf. However, for recent disagreements with Almond’s argument, see Brown R.: The 1918 US Influenza Pandemic as a Natural Experiment, Revisited. Unpublished seminar paper, February 2011, available at: http://dupri.duke.edu/pdfs/ryanbrownpaper.pdf; and Cohen, A. A., Tilinghast J. and Canudas-Rono V.: No Consistent Effects of Prenatal or Neonatal Exposure to Spanish Flu on Late-life Mortality in 24 Developed Countries: in Demographic Research, 22, 20 (2010), pp. 579-634
- ↑ Anonymous caller on SAFM radio programme, Talk at Will, 16 September 1998.
- ↑ Transcript of interview with William Maxwell in: American Experience: Influenza 1918, PBS 1998, available at: www.pbs.org/wgbh/americanexperience/features/transcript/influenza-transcript/
- ↑ Cited in Phillips: Black October, p. 188 (translation from Dutch by the author).
- ↑ Johnson: Britain and the 1918-19 Influenza Pandemic, p. 161.
- ↑ Echeverri, Beatriz: Spanish Influenza Seen from Spain, in: Phillips and Killingray (eds): The Spanish Influenza Pandemic of 1918-19, p.173.
- ↑ Cited in Phillips, Black October, p. 150.
- ↑ Ibid.
- ↑ Ibid., p. 141.
- ↑ Ibid., p. 149.
- ↑ Bristow, American Pandemic, p. 195.
- ↑ Kent, Susan K.: Aftershocks: Politics and Trauma in Britain, 1918-1931. Basingstoke 2009, p. 4.
- ↑ Cited in Phillips: Black October, p. 133.
- ↑ Smallman-Raynor, Matthew R. and Cliff, Andrew, D.: War Epidemics. An Historical Geography of Infectious Diseases in Military Conflict and Civil Strife, 1850-2000, Oxford 2004, p. 580.
- ↑ Cited in Rice, Geoffrey W.: Black November. The 1918 Influenza Pandemic in New Zealand, Christchurch 2005, p. 95.
- ↑ Cited in Phillips: Black October, p. 190.
- ↑ Sources for these figures: Crosby: Epidemic and Peace, 1918, p. 159; Byerly, Carol R.: Fever of War. The Influenza Epidemic in the US Army During World War I , New York 2005, p. 99; Price-Smith, Andrew T.: Contagion and Chaos. Disease, Ecology, and National Security in the Era of Globalization, Cambridge, Massachusetts 2009, pp. 67, 71; Butler, A. G.: The Australian Army Medical Services in the War of 1914-1918, volume 3, Melbourne 1943, p. 196; Mitchell, T. J. and Smith, G. M.: Medical Services. Casualties and Medical Statistics of the Great War, London 1931, pp. 86, 167; Macpherson, W. G. et al: Medical Services. Diseases of the War, volume 1, London 1922, pp. 174-176; Harrison, Mark: The Medical War. British Military Medicine in the First World War, Oxford 2010, p. 141; Michels, Eckard: Die Spanische Grippe 1918/19. Verlauf, Folgen und Deutungen in Deutschland im Kontext des Ersten Weltkriegs in: Vierteljahrshefte für Zeitgeschichte, 58, 1 (2010), p. 14; Erkoreka: Origins of the Spanish Influenza Pandemic, p. 192; Lahaie: L'épidémie de grippe dite “espagnole”, p. 14; Parsons, W. D.: The Spanish Lady and the Newfoundland Regiment: at www.gwpda.org/medical/parsons.htm
- ↑ Cited in Lahaie: L'épidémie de grippe dite “espagnole”, p. 104, n. 45.
- ↑ Cited in Johnson, John Henry: 1918. The Unexpected Victory, London 1997, p. 192.
- ↑ Cited in Fasse, Alexander: Im Zeichen des „Tankdrachten“. Die Kriegführung an der Westfront 1916-1918 in Spannungsverhältnis zwischen Einsatz eines neuartigen Kriegsmittels der Alliierten und deutschen Bemühungen um seine Bekämpfung, Dr phil thesis, Humboldt University, Berlin 2007, p. 258. Available at http://edoc.hu-berlin.de/dissertationen/fasse-alexander-2007-06-21/HTML/chapter10.html&prev=/search%
- ↑ Cited in Johnson, Britain and the 1918-19 Influenza Pandemic, p. 188.
- ↑ Cited in Herwig, H. H.: The First World War. Germany and Austria-Hungary 1914-1918, London 1997, p. 417.
- ↑ Cited in Strachan, Hew: The First World War. New York et al. 2003, p. 315.
- ↑ Kitchen, Martin: The Silent Dictatorship. The Politics of the High Command under Hindenburg and Ludendorff 1916-18, London 1976, p. 254.
Selected Bibliography
- Åman, Margareta: Spanska sjukan. Den svenska epidemin 1918-1920 och dess internationella bakgrund (The Spanish Influenza. The Swedish epidemic, 1918-1920, and its international background), Uppsala 1990: Ubsaliensis Academiae.
- Barry, John M.: The great influenza. The epic story of the deadliest plague in history, New York 2004: Penguin.
- Bertolli Filho, Cláudio: A gripe espanhola em São Paulo, 1918. Epidemia e sociedade, Santa Ifigênia, São Paulo, SP 2003: Paz e Terra.
- Blakely, Debra Ellen Menconi: Mass mediated disease. A case study analysis of three flu pandemics and public health policy, Lanham 2007: Lexington Books.
- Bristow, Nancy K.: American pandemic. The lost worlds of the 1918 influenza epidemic, Oxford; New York 2012: Oxford University Press.
- Byerly, Carol R.: Fever of war. The influenza epidemic in the U.S. Army during World War I, New York 2005: New York University Press.
- Crosby, Alfred W.: America's forgotten pandemic. The influenza of 1918, Cambridge; New York 2003: Cambridge University Press.
- Echeverri Dávila, Beatriz: La gripe española. La pandemia de 1918-1919, Madrid 1993: Centro de Investigaciones Sociológicas.
- Erkoreka, Antón: La pandemia de gripe española en el País Vasco (1918-1919), Bilbao 2006: Museo Vasco de Historia de la Medicina y de la Ciencia.
- Foley, Caitriona: The last Irish plague. The great flu epidemic in Ireland 1918-19, Dublin 2011: Irish Academic Press.
- Hartesveldt, Fred R. van (ed.): The 1918-1919 pandemic of influenza. The urban impact in the Western World, Lewiston 1992: E. Mellen Press.
- Humphries, Mark Osborne: The last plague. Spanish influenza and the politics of public health in Canada, Toronto; Buffalo 2013: University of Toronto Press.
- Johnson, Niall: Britain and the 1918-19 influenza pandemic. A dark epilogue, London; New York 2006: Routledge.
- Jones, Esyllt Wynne: Influenza 1918. Disease, death, and struggle in Winnipeg, Toronto; Buffalo 2007: University of Toronto Press.
- Killingray, David / Phillips, Howard (eds.): The Spanish influenza pandemic of 1918-1919. New perspectives, London 2013: Routledge.
- Müller, Jürgen: 'Die Spanische Influenza 1918/19. Der Einfluβ der Ersten Weltkrieges auf Ausbreitung, Krankheitsverlauf und Perzeption einer Pandemie', in: Eckart, Wolfgang Uwe / Gradmann, Christoph (eds.): Die Medizin und der Erste Weltkrieg, Pfaffenweiler 1996: Centaurus-Verlagsgesellschaft.
- Phillips, Howard: Black October. The impact of the Spanish Influenza epidemic of 1918 on South Africa, Pretoria 1990: Government Printer.
- Price-Smith, Andrew T.: Contagion and chaos. Disease, ecology, and national security in the era of globalization, Cambridge 2009: MIT Press.
- Rice, Geoffrey / Bryder, Linda: Black November. The 1918 influenza pandemic in New Zealand, Christchurch 2005: Canterbury University Press.
- Shanks, G. Dennis, International Society for Influenza and other Respiratory Viruses Diseases (ed.): 'Low but highly variable mortality among nurses and physicians during the influenza pandemic of 1918-19', in: Influenza and other respiratory viruses 5/3, 2011, pp. 213-219.
- Smallman-Raynor, Matthew R. / Cliff, Andrew: War epidemics. An historical geography of infectious diseases in military conflict and civil strife, 1850-2000, Oxford 2004: Oxford University Press.
- Witte, Wilfried: Tollkirschen und Quarantäne. Die Geschichte der Spanischen Grippe, Berlin 2008: Wagenbach.