The Shell-Shocked Soldier↑
In 1916 a young Australian soldier was admitted to Seale Hayne hospital in Devon from where he wrote the following letter to his family:
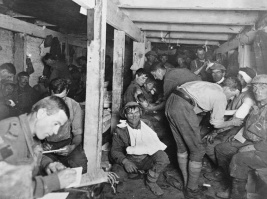
The soldier was suffering from shell shock. In his case the symptoms were hysterical deafness and loss of speech, conditions which were treated with a single dose of ether. Doctors told him in writing that it would restore his speech and hearing. He initially struggled but after a few whiffs he whispered "mother". He "then repeated it louder and louder until he shouted with a voice that would have filled the Albert Hall." Once his voice and his hearing returned the associated conditions – depression, headaches and insomnia – disappeared too.[2]
Arthur Hurst (1879-1944), a neurologist and commanding officer at Seale Hayne told this story to demonstrate wartime psychiatry at its most successful. The soldier, an ordinary man from the ranks, had broken down during active combat and so he had nothing to be ashamed of. In addition he had faith in the doctors who were his social and military superiors and he responded well to treatment. Like many others in this situation his first words were indicative of his moral character: in doctors’ descriptions men recovering their voices generally called for their mothers, sang the national anthem or declared "God Save the King!"
By 1916, the military medical professions of all combatant armies were developing ways of managing mentally wounded soldiers.[3] Men have long broken down in wars but it was not until the First World War that mental breakdown amongst troops presented a significant problem in terms of morale and manpower. Given the nature of war neurosis it is difficult to estimate accurately the numbers of men that were affected. There were over 80,000 recorded cases amongst the British armies on the western front; estimates amongst German troops range from 200,000-300,000 and the number of French troops affected was similar or possibly higher.[4] The statistics identify horrific numbers of traumatised men but war neuroses accounted for only a relatively small percentage of battle casualties overall.[5] Nevertheless medical officers at the time felt overwhelmed by the "extraordinary incidence of mental and functional nervous diseases": the numbers of mentally wounded were unprecedented by comparison with previous wars, and shell shock affected military morale and discipline "in a special way."[6] It is this "special" nature of First World War shell shock that has provoked such widespread interest in the subject, as the treatment of military mental breakdown has provoked questions about madness, class, masculinity, medical progress and military discipline. As a result the history of First World War shell shock is broad and includes the history of mental trauma per se, the history of shell shock as a specific military medical condition and its social and economic consequences, and the history of shell shock as an emblem or a metaphor for the war and its aftermath.
Shell Shock and History↑
There was much medical commentary on shell shock during and immediately after the war yet historians paid little attention to its history until the late 1970s when Eric Leed argued that shell shock was a soldier’s flight from ‘intolerable reality’ and that neurosis provided men with a legitimate – if temporary – respite from the rigours of warfare.[7] This was the first of numerous studies into military medicine and ethics. The recognition of Post-Traumatic Stress Disorder (PTSD) in 1980 prompted historians and medical experts to situate modern trauma in its historical context.[8] This attention to the history of war neuroses was matched by a growth in the longer-term histories of shell-shocked men and their families, many of whom had to deal with the emotional impact of the war for years, or even decades, after the armistice.[9]
In Britain there has long been an extensive historical, political and cultural interest in shell shock.[10] The topic does not have the same popular resonance in Germany: nevertheless there is a substantial history of German wartime and post-war psychiatry. Paul Lerner’s seminal work indicates the extent to which the history of modern German psychiatry has long been seen through the prism of the Third Reich. Yet to understand early 20th century war psychiatry we need to abandon this teleological narrative and focus instead on the political, economic and cultural debates of Wilhelmine Germany because it was the social legislation of the Second Reich which meant that neurotic soldiers were treated in the same way as injured industrial workers.[11] Turning to the post-war world, Jason Crouthamel highlights the tensions surrounding the treatment of war neurotics as rival political groups tried to appropriate mentally wounded veterans for their own causes.[12] In France, Sophie Delaporte opened up the study of French shell shock, ensuring that trauma became crucial to the wider understanding of the First World War.[13] Gregory Thomas’ extensive history investigates the effect of war neuroses on soldiers, civilians, and medical professionals but shell shock is still a comparatively under-researched subject in France, despite a growing interest in the history of the war itself.[14]
A number of historians have recently incorporated the psychologically wounded into the wider medical history of the First World War, yet there has been no European survey of the history of shell shock.[15] In response, this article offers a brief synthesis of combatant trauma throughout Europe. The focus is on the soldiers of the primary combatant nations on the western front because although men were traumatised in all areas, the conditions on the western front were unique, being characterised by highly industrial, intensive and static trench warfare. In consequence, the type of "mental cases" seen on the western front were not replicated in all sectors.[16]
Doctors and Shell Shock: Early Responses↑
The first mental casualties appeared after the Battle on Mons in 1914 and they portrayed a baffling range of symptoms: tics, trembling, functional paralysis, hysterical blindness and deafness, speech disorders ranging from stuttering to mutism, confusion, extreme anxiety, headaches, amnesia, depression, unexplained cramps, fainting and vomiting. It had long been understood that strong nerves would be required to fight a modern industrial European war. Wilhelm II, German Emperor (1859-1941) had declared that victory would go to the nation with "strongest nerves" – yet many German doctors believed that war would provide "cathartic front experiences" that would actually strengthen enfeebled, degenerate modern men.[17] Similarly, many French doctors believed that the war would revitalise individual Frenchmen as well as French science and medicine.[18] The sense of war as a tonic was strongest amongst the German psychiatric profession but was also present in Britain where doctors routinely extolled the virtues of "character."[19]
In retrospect doctors were able to argue that the First World War produced "no new symptoms".[20] Yet doctors dealing with mentally traumatised soldiers often felt that they were facing completely unprecedented problems. Lieutenant Colonel Charles Myers (1873-1946) anthropologist and consulting psychologist to the British Expeditionary Force first publicly used the term "shell shock" in The Lancet in February 1915.[21] The term implied a direct link between a bursting shell and trauma, a diagnosis that was as emotionally satisfying as it was medically imprecise, as Myers quickly recognised. Consequently, British medical and military authorities tried in vain to proscribe the term and to find a suitable alternative. In 1917 Medical Officers were instructed to label possibly traumatised men as NYDN (Not Yet Diagnosed Nervous) but throughout the war, and afterwards, men continued to be described as "shell-shocked" and a wide range of other terms were used too: hysteria, neurasthenia, hybrid hystero-neurasthenia, nerve shock, war shock, war neurosis, exhaustion. Closer to the front line, doctors’ private papers sometimes simply refer to men as "mental cases" or even "dotty".[22] There is no direct translation for the Anglo-Saxon "shell shock" but there was a similar variety of descriptions in other European armies.[23] The French discussed commotion cerebrale, accidents nerveux, and obusite ("shellitis"). French commotionnés were most commonly diagnosed with hysteria and tended to be described as suffering from "mental confusion".[24] German medics referred to Kriegneurosen and Krieghysterie, and sufferers were popularly referred to as Kriegszitterer (war quiverers) or Schüttler (shakers). The Italians referred to shock da esplosione emphasising the importance of the physical shock. Thomas Salmon, who had been commissioned to observe the British treatment of shell shock for the US army, commented that "it is doubtful if there is another group of diseases in which more confusion in terms exists."[25]
War psychiatry does not develop in isolation from civilian psychiatry and throughout the war military psychiatry drew from concepts in the civilian world where there had been much medical investigation into mental trauma since the late 19th century.[26] Shell shock may have appeared to be a new condition, requiring a new language but responses to mentally traumatised, apparently hysterical soldiers were all rooted in the debates, cultural assumptions and practices of the pre-war period. The violence of the modern, industrial world was provoking anxiety long before the outbreak of the First World War. Passengers and workmen involved in railway accidents often suffered from odd symptoms such as partial paralysis, headaches, backache, dizziness and loss of memory, none of which seemed directly related to the initial impact or physical shock. While it was accepted that "railway spine" could be explained by damage to the central nervous system, there was also some debate about the extent to which it had been caused by "fright alone".[27] "Neurasthenia" was also coined in this period. In 1869 George Beard (1839-1883), an American physician and neurologist, used the term to describe patients suffering from a range of physical and mental symptoms such as headaches, impotence, anxiety, paralysis, neuralgia, depression and loss of memory. He attributed neurasthenia to the nerve damage caused by the strain of modern, highly competitive, urban life. As a result of its association with modernisation sufferers were not stigmatised and were often treated with Silas Weir Mitchell’s (1828-1914) "rest cure". A modified version of this cure was later adapted to treat British officers during the First World War.
Railway spine and neurasthenia affected men and women alike but hysteria has traditionally been considered a specifically female complaint. In France, the acclaimed neurologist Jean-Martin Charcot (1825-1893) published widely on traumatic hysteria, indicating that it was not a malady appertaining only to women and to effete men: his male patients were workers, artisans and peasants.[28] However despite this nuanced understanding of male hysteria, the subject was barely mentioned in medical textbooks, encyclopaedias or dictionaries.[29] On the whole hysteria remained "a female malady".[30] Yet hysteria was also a class-bound diagnosis and since the late 19th century German psychiatrists had used it to pathologise "work-shy" working-class men.[31] In Britain the situation was similar and so during the war it became normal practice to categorise traumatised officers as neurasthenic and in need of rest and recuperation whereas men from the ranks were more likely to be labelled as hysterical and treated more harshly.[32] Despite official proclamations insisting that these "unfortunate men would not be treated like ordinary lunatics", many men with hysterical symptoms did feel that they were punished and incarcerated rather than treated.[33]
In both war and peace the psychiatrist’s role remains the same, namely to diagnose and to treat the mentally disturbed patient and to further scientific knowledge through clinical observation. In addition, psychiatrists had their own political and professional aims, and many doctors were enthusiastic about the professional opportunities offered by the war. German doctors thought of the war as a great "experiment", similarly their French counterparts saw it as "a grandiose laboratory experiment".[34] However, the comparison fell short because laboratory experimentation implies order and a level of control which was not always possible in wartime, especially close to the fighting zones. First, men were not always treated by mental-health specialists, especially in the early stages of the war. In addition, doctors continually complained about the difficulty of collecting statistics, monitoring cases and maintaining dialogue with colleagues. Doctors working at the Salpêtrière in Paris admitted that some of their methods were "makeshift", and some Italian medics even abandoned all correlation between diagnosis and treatment.[35] At the same time, war psychiatrists were faced with more than just practical difficulties as the conditions of war served to deepen, rather than alleviate, some key pre-war anxieties. Fin de siècle psychiatry had developed amongst fierce concerns about national degeneracy and a strong belief in social Darwinism. Yet the belief that only fit societies would survive was combined with growing fears that relentless trench warfare was producing a dis-eugenic war, one in which the least fit were destined to survive. This provoked already entrenched fears of "pension neurosis" or even outright fraud.[36] The belief that the financial security of a pension would encourage a man to maintain rather than discard his neurotic symptoms continued as a source of political friction and social resentment throughout the inter-war years.
The practical arrangements for shell-shocked casualties varied across sectors and developed in response to the exigencies of warfare and to the professional goals of the medical profession. British and German troops were initially sent home for treatment but the French – fighting on their own territory – were less able to send men away from the firing lines and so developed treatment centres closer to the front.[37] By the summer of 1917 each French army had its own neurological centre, with approximately 200 beds, about fifteen miles from the front, and these were supported by regional neurological bases and psychiatric centres further to the rear. All neurological cases were directed to the forward centres in the first instance because specialists wanted to deal with mental complaints before they became intractable.[38] Influenced by the French example, Myers insisted on forward centres in the British zones. The military command was initially hostile but forward treatment soon became standard practice amongst the western allies.[39] The approach of the Central Powers was different. The German armies continued to send troops back to Germany where they were generally treated in large hospitals although work-based therapies were developed in Germany from 1915.[40] In stark contrast, the Austro-Hungarian armies centralised their treatment in Vienna and by the end of the war there were approximately 120,000 shell-shocked soldiers in the capital.[41] The Austro-Hungarian approach was unique as throughout Europe mentally wounded soldiers were generally hidden or dispersed – in Britain "mental cases" were often not unloaded with the physically wounded men but were held in separate railway carriages and quietly spirited away to remote locations, far from the gaze of onlookers or even ordinary nursing staff.
Shell Shock, Cowardice and Discipline: the Ethics of Military Mental-Medicine↑
"Can war make any man a coward in time?" asked Charles McMoran (1881-1977), later Lord Moran, a renowned physician who served in both world wars.[42] This question lay behind much military medical treatment because doctors were dealing with men who would not or could not fight, despite the lack of an obvious physical wound. Moran eventually concluded that all men had a limited stock of courage and that "men wear out in war like clothes" but not all medics agreed.[43] Frederick Walker Mott (1853-1926) dismissed some of the shell-shocked as simply "shell-shy", a term every bit as disparaging and dismissive as the "work-shy" label which had been applied to the pre-war working class, and many doctors would have concurred with Marc Bloch’s (1886-1944) rather contemptuous dismissal of a French corporal as a "neurasthenic man of the world, not much of a warrior".[44] Most doctors wholeheartedly supported the war aims of their respective nations and also accepted that self-respecting, healthy males should make effective soldiers.
The relationship between serving soldiers and their medical officers is not always straightforward. Doctors can be seen as the humane, civilising face of warfare: the International Red Cross had organised medical care so as to humanise warfare and some pacifists, while eschewing military combat, accepted military medical service.[45] Yet the belief that doctors were primarily committed to their own armed services – and to their own career advancement – often provoked antagonism from ordinary soldiers. In the doctor-patient relationship the power is tilted towards the doctor and during wartime this asymmetrical power relationship was weighted even more heavily in the doctor’s favour because doctors were medical officers and therefore senior in rank – and also in class – to most soldier patients. As a result, soldiers from the other ranks were often hostile to medical officers and this hostility was especially rife in cases of war neuroses where a neurologist, psychiatrist or even a doctor without specialist training could withhold treatment rights, deny a pension or sanction disciplinary action. For these reasons men in the trenches often tried to avoid sending a mentally wounded man to see a doctor. In 1916 a British soldier in the trenches was stricken dumb with fear. Recognising the loss of speech as an hysterical symptom, his comrades slapped him, tickled him and poured boiling tea over him to make him shriek.[46] This ad hoc treatment may seem absurd but its purpose was to restore the man’s speech and spare him from the medical professionals: it tells us much about the ordinary soldier’s faith in wartime psychiatry.
The language of cowardice permeates the wartime discourse and even in its absence doctors assumed that war neurosis arose in men who were predisposed to some kind of mental breakdown and were therefore flawed, if not culpable. Yet although doctors shared these basic assumptions the range of treatments was diverse. First responses often encouraged rest on account of the links between shell shock and physical and mental exhaustion. A British stationary hospital in France simply encouraged men to stay in bed for three or four days and German soldiers were also given "soft" therapy in the form of spruce needle baths, good food and valerian.[47] More focused or active therapies could include re-education, hypnosis, intensive massage or hydrotherapy. These treatments were all designed to re-awaken the afflicted senses and demonstrate to the patient that he still had control of his physical faculties. The ether given to the young Australian at Seale Hayne was to relax him so that he would be more suggestible, and ether often accompanied light hypnotism.[48] Re-education could be benign – it included singing lessons for men with speech disorders – but it could also appear harsh. Hurst describes trying to awaken a man suffering from hysterical deafness by banging a poker on a coal scuttle at his bedside – a type of treatment very similar to that carried out by the ordinary Tommies in the trenches.[49] In contrast, a limited range of practices were inspired by psycho-analytic theory. William Rivers (1864-1922) has become famous for the "talking-cure" at Craiglockhart, a British hospital for officers, and there were also attempts to promote dream therapy in men from the other ranks in the Red Cross hospital at Maghull.[50] Men resisted the dream therapy, which they perceived as intrusive, but they were most visibly opposed to harsh physical treatments which seemed little short of punitive.
It is electro-shock therapy, known as the Kaufmann treatment in Germany and Austria, which has become the most notorious of shell-shock treatments. The Hamburg neurologist and wartime psychiatrist Professor Max Nonne (1861-1959) required his patients to be naked during treatment to increase their vulnerability, as did many doctors in France.[51] In Britain Lewis Yealland’s (1884-1954) electrotherapy evoked disquiet not just from ordinary soldiers but from other doctors who worried that the over-use of simple electrotherapy would condemn patients to the care of untrained "medical electricians".[52] Proponents of electric shock therapy argued that it worked and that it was not necessarily inhumane.[53] Yet whatever its merits, soldiers were frightened of it and protests demonstrate the extent to which patients and the general public wanted to curtail the excessive power of wartime psychiatrists. In May 1916, Baptiste Deschamps (1881-1953), an ordinary soldier in the French army, was sent to Dr Clovis Vincent’s (1879-1947) neurological centre for treatment. As the electric treatment was beginning, a clearly terrified, and possibly furious, Deschamps punched Vincent, an action punishable by death. Deschamps was tried and found guilty of having assaulted a superior officer but was only given a suspended sentence of six months in prison.[54] The case provoked a great public outcry in Deschamps’ favour and, despite the power of the military medical profession, the tribunal was forced to treat him leniently.
Not all doctors were quick to brand shell-shocked men as cowards or to treat them as criminals. In July 1916, a party from an infantry battalion failed to carry out a raid on their sector of the western front. The officer in charge called for the medical officer, Lieutenant George Kirkwood (1879-1931), who later issued a certificate testifying to collective mental breakdown amongst the men:
Kirkwood was promptly disciplined and removed from his post because his sympathy with the men ran counter to military discipline. Doctors had constantly to balance clinical and military requirements and could be punished either for excessive harshness or excessive leniency. In Kirkwood’s case the question of discipline was overt but it could be subsumed into more complex clinical debates. This was especially notable in Germany where battles within the medical profession led to the diagnosis of traumatic neuroses being replaced with that of hysteria.
In Wilhelmine Germany, Hermann Oppenheim (1858-1919) had demonstrated that traumatic events were pathogenic and could provoke post-traumatic neuroses. This thesis had been accepted by the Imperial Insurance Office in 1889 and German workers were entitled to compensation if they developed neurotic symptoms after an accident. Yet some medical professionals suspected "pension neurosis" amongst the feckless working class and preferred instead to diagnose "hysteria", a label implying both predisposition and weakness of will. Conflict continued until the 1916 War Neurology Congress in Munich when Oppenheim was isolated and roundly defeated. Elite psychiatrists and neurologists rejected Oppenheim’s diagnosis of neuroses but non-specialists – and certainly the lay public – accepted the notion that the war caused nervous or mental illness. This medical debate had significant political implications. Military psychiatrists were firmly of the belief that war neurotics were malingerers, degenerates or frauds and that awarding them a pension would only encourage their symptoms.[56] In consequence the psychiatric profession – already aligned with the establishment before the war – became closely associated with the highly punitive military state and the old elites. It was therefore firmly at odds with the Social Democratic state of the early Weimar years and mentally wounded soldiers’ efforts to win effective pensions became politically contentious and remained so throughout the Weimar Republic. War psychiatrists became targets for fierce anger, especially from working-class veterans and their families.
Shell Shock after the War: Pensions and Politics↑
The problem of shell shock did not end with the armistice. Some men succumbed to nervous collapse after hostilities had ceased; some appeared to get better and then suffered from relapses. Moreover, the war wounded and their families, in both victor and combatant nations, wanted some kind of recompense. Notions of citizenship varied across Europe but the men who had fought in the Great War believed that they had a right to state support: the "thanks of the fatherland" meant little without money and access to health care.[57] The British government introduced a statutory pension scheme for veterans in 1915 and did award pensions for neuroses, however the bureaucratic process was cumbersome, the final awards were meagre and there were many complaints about care and conditions in Ministry of Pension Hospitals.[58] The situation was similar in Germany where veterans with nervous disorders accounted for almost half of all military pension claimants.[59] The 1920 National Pension Law did accord pension rights to psychologically disabled veterans whose injuries were directly attributable to war service, although a 1926 ruling removed these rights on the basis that men who were still disturbed so long after the war were clearly not suffering from a war-related wound.[60] In France war hysterics received no pension unless they were so incapacitated that they required internment, at which point they had to use their paltry pensions to pay asylum fees.[61] Interned, mentally wounded veterans, known as "les morts-vivants", had little political support and were often deeply isolated. As if to emphasise this metaphorical death the wives of aliénés received the equivalent of a widow’s pension.[62] The disparity between physically and mentally wounded veterans generated much anger, and although French pension rates were revised in 1929, the psychologically wounded veteran remained far worse off than his physically wounded counterpart. Impoverished war neurotics remained a standard feature of daily life throughout inter-war Europe. Paintings by Otto Dix (1891-1969) and George Grosz (1893-1959) are characterised by Kriegszitterer on street corners; George Orwell (1903-1950) noted the tormented shrieks of shell-shocked men in tramps’ hostels in the 1930s.[63] More obliquely, the trauma of the war looms large in post-war film and in the avant-garde art world, notably in Dada, German expressionism and Surrealism.[64]
In addition to this underlying discontent, the treatment of war neurotics continued to provoke high-profile political scandals in the post-war years. In Britain concerns about shell shock were dominated by two issues: lunatic asylums and courts-martial. Soldiers suffering from shell shock should not have been labelled as insane and should not have been sent to lunatic asylums, nevertheless many of them were and they were often placed some distance from their homes, making family support difficult, if not impossible. In addition, lunatic asylums were popularly known as pauper lunatic asylums because they were traditionally populated by those unable to afford a private clinic. That the government later agreed to pay for service patients to be treated as private patients was largely irrelevant: ex-servicemen and their families deeply resented the twin stigmas of insanity and poverty. In response, the Ex-Services’ Welfare Society (ESWS), initially established by the wives of shell-shocked men, campaigned on behalf of veterans in asylums throughout the 1920s. The ESWS provoked government ire by insisting that veterans languished in asylums but also attracted popular support by providing dignified, non-institutional care for mentally wounded men.
Concerns about courts-martial were based on the fear that "through inadvertence and want of knowledge, dreadful things may have happened to unfortunate men who had in fact become irresponsible for their actions".[65] In response, Francis Hopwood, Lord Southborough (1860-1947) was charged with chairing the official Government Committee of Enquiry into Shell Shock in 1920. The committee did not re-open any courts-martial cases, rather it focused on identifying the causes of shell shock and on highlighting appropriate responses. The outcome, after two years of enquiry, was ambiguous. While acknowledging that men could suffer mental collapse as a result of the strains of war it also insisted upon the importance of predisposition; while recognising that shell-shocked men should be properly treated, contributors concluded that treatment should be based on military experience and common sense rather than medical knowledge, as the following comments attest:
Wartime mental-health specialists had clearly not made themselves appear indispensable in the British army. Moreover, the belief that war could regenerate weak men endured. Emanuel Miller (1892-1970) described a previously "timid" man who had become a respected soldier on the western front and noted that "several instances have come under observation of decorations for bravery that have been won under the occurrence of 'shell shock'".[67] The conviction that a shell-shocked man could go to fight another day could lead to a lack of sympathy for a man suffering from a relapse yet the belief in recovery also ensured that shell shock was not necessarily shameful, especially if the man had "done his bit". In consequence, British post-war images of shell-shocked men could successfully present them as both hard-working and respectable.
The Southborough committee did not manage to allay concerns about the mental health of servicemen who had been executed and the issue resurfaced at the end of the 20th century when their families demanded an official pardon. Central to their argument was that the medical profession should have recognised the symptoms of shell shock and that men had been unjustly punished for the failures of wartime psychiatry.[68] In contrast, public concern about the French fusillés was not expressed in the same medicalised discourse. For those on the political left, the fusillés were "martyrs to the radical pacifist position": they had died because they had taken the honourable stance and had refused to fight, not because they had lost their reason.[69] The French fusillés were heroic in a way that the shell-shocked poilu was not; in Britain these two identities converged and the shell-shocked soldier became a very particular sort of hero, namely the hero-victim, best exemplified by the fictional Harry Penrose, a young officer shot for cowardice. The character of Penrose in the novel The Secret Battle was a clear indictment of the military system that destroyed men’s nerves and then punished them for it. Moreover, it was a characterisation that provoked widespread sympathy even amongst conservative political elites, with Winston Churchill (1874-1965) describing Penrose as a "gallant soldier" who had been "caught in the teeth of the military machine".[70]
Post-war anger also motivated a committee of investigation into shell-shock treatment in Austria, in this case, the specific use of electrotherapy. In the autumn of 1920 Julius Wagner-Jauregg (1883-1940), Professor of Psychiatry at the University of Vienna, was accused of treating soldier patients brutally with electric currents. Individual patients had resisted treatment during the war and there were even patient revolts in some hospitals. As a result, Wagner-Jauregg and six others had to justify their use of electrotherapy in court. Here there are clear parallels with the case of Vincent and Deschamps in France but there are also important racial differences. The German-speaking medical elite was often suspicious of the "foreign-speaking" soldier patients in the multi-ethnic Austro-Hungarian armies. Unlike hypnosis or suggestion therapy, electric treatment was a way of exposing malingerers with only limited recourse to language: it could be a virtually "speechless therapy".[71] Of course ethnic-focused psychiatry was not limited to the Austro-Hungarian Empire. The British authorities insisted that troops from southern Ireland were especially prone to mental weakness; the German authorities had similar attitudes towards Jews in the German army; French specialists perceived black troops, especially those from Senegal, as especially prone to psychiatric disorders.[72]
High-profile anxieties about patient treatment existed alongside a growing suspicion of shell-shocked men in the post-war period. The wartime belief that war neurotics were faking, malingering or exaggerating was never fully dispelled, rather it became more pronounced as time went by and it grew more difficult to make direct links between a man’s wartime experience and his post-war mental state. "Are you a potential post-war criminal?" a popular magazine asked its readers, before going on to list the crimes and anti-social behaviour associated with shell shock.[73] The politicised nature of military medicine and the diverse and paradoxical attitudes towards shell shock ensured that the condition – and shell-shocked veterans – became a politically potent tool in post-war Europe. This was most obvious in the new Weimar Republic which was scarred by the defeat of war and continually marred by political violence. The fledgling welfare state, initially established by the Social Democratic Party (SPD), should have ensured adequate health care and pensions for psychologically damaged veterans. In the early 1920s the SPD saw war neurosis as a universal experience that was shared by all German citizens and so could unite the post-war Volksstaat. Yet this unity was far from realised. Men who had fought resented being categorised alongside women and civilians whose wartime stresses had been limited to the home front; the welfare system was administered by cost-cutting officials in the Labour Ministry; the whole process relied upon the advice of psychiatrists, most of whom were highly conservative nationalists who blamed weak or degenerate men for losing their nerve in 1918 and bringing Germany to defeat and revolution. As a result men did not find it easy to access support and the situation grew worse as pensions were cut throughout the 1920s.[74]
The SPD failed the psychologically damaged veterans they sought to protect and state welfare was inadequate. Their opponents further to the left – the German Communists (KPD) – had never believed that the bourgeois state could serve the needs of the working-class soldier and was most vocal in attacking the highly conservative psychiatric establishment. As far as the KPD was concerned, the state-hired psychiatrist was no more than "a businessman disguised as a doctor" and, like all members of the ruling class, it was in his interest to deny the trauma of the last war so as to prepare the proletariat for yet another one.[75] Where did the shell-shocked veteran fit into these political arguments? While many shared the KPD’s hostility to doctors, they could draw little comfort from its solutions. KPD activists were opposed to state-sponsored welfare measures which they saw as turning men into helpless dependants, and they argued that neurotic men needed to "find healing in active class struggle and revolution", not handouts from the bourgeois state.[76] There is a peculiar parallel between KPD opposition to pensions and the approach of the conservative and the extreme right. Conservative doctors castigated the Weimar welfare state for "coddling" neurotics with pensions, and Nazis were similarly hostile because the very existence of war neurotics challenged the Nazi glorification of the war experience. In consequence, the National Pension Law of 1934 cut off all pensions for mentally disabled veterans.[77] Throughout these battles – and against the odds – German veterans of all political persuasions continued to petition for pension rights and insisted that they should be treated with the same dignity as their physically wounded comrades.
Conclusions: Hero-Victims and Patient Protest↑
The history of wartime and post-war shell shock is both ambiguous and paradoxical. During the war medical officers, soldiers and civilians displayed sympathy and understanding to shell-shock victims in all combatant armies. At the same time the military code prevailed, as did the medical belief in predisposition and the importance of will; some military medics were hostile to the very idea of war neurosis. As a result wartime medicine was often found wanting and could be described as more disciplinary than therapeutic. After the war many shell-shocked men were forgotten or discredited, or – in Britain – became idealised hero-victims. The political issues provoked by shell shock varied across Europe but all of the issues which made shell shock politically important – courts-martial, lunatic asylums, electrotherapy, pension disputes – indicate the extent to which shell-shock treatment was constantly entwined with discipline. Yet shell-shocked men were not simply victims of total war, mental collapse and punitive treatment regimes. Both during the war and afterwards, formally and informally, patients and their families consistently demanded proper treatment and adequate pensions. They did not always succeed but men refused to be stigmatised by a mental war wound: the history of shell shock is a history of trauma and psychiatry but it is also history of patient protest.
Fiona Reid, Newman University
Section Editors: Michael Neiberg; Sophie De Schaepdrijver
Notes
- ↑ Wellcome Library, London (hereafter W.L.): Hurst, Arthur: Twentieth Century Physician: Being the Reminiscences of Sir Arthur Hurst DM, FRCP, London 1949, p. 170.
- ↑ Ibid., p. 171.
- ↑ For documents on the medical history of the war see http://www.vlib.us/medical/ (retrieved: 28 February 2013).
- ↑ Stone, Martin: Shellshock and the Psychologists, in: Bynum, William F. / Porter, Roy / Shephard, Michael (eds): The Anatomy of Madness. Essays in the History of Psychiatry Volume II, London 1985, p. 249; Lerner, Paul: From Traumatic Neurosis to Male Hysteria, in: Micale, Mark and Lerner, Paul (eds): Traumatic Pasts. History, Psychiatry and Trauma in the Modern Age, 1870-1930, Cambridge et al. 2001, p. 141; Crouthamel, Jason: The Nation’s Leading Whiner. Visions of the National Community from the Perspective of Mentally Traumatized Veterans, in: Hofer, Hans-Georg / Prüll, Cay-Rüdiger / Eckart, Wolfgang U.: War, Trauma and Medicine in Germany and Central Europe (1914-1939), Freiburg 2011, p. 75; Roudebush, M.: A Battle of Nerves. Hysteria and its Treatments in France during World War I, in: Micale and Lerner, Traumatic Pasts 2001, p. 254.
- ↑ Harrison, Mark: The Medical War. British Military Medicine in the First World War, Oxford 2011, p. 110.
- ↑ Salmon, Thomas: The Care and Treatment of Mental Diseases and War Neuroses (“Shell Shock”) in the British Army, in: Mental Hygiene 1/4 (1917), p. 509.
- ↑ Leed, Eric J.: No Man’s Land. Combat and Identity in World War One, Cambridge 1979, p. 168.
- ↑ Shephard, Ben: A War of Nerves. Soldiers and Psychiatrists in the Twentieth Century, London 2000; Jones, Edgar and Wessely, Simon: Shell Shock to PTSD. Military Psychiatry from 1900 to the Gulf War, Hove et al. 2005.
- ↑ Barham, Peter: Forgotten Lunatics of the Great War, New Haven et al. 2004; Reid, Fiona: Broken Men. Shell Shock Treatment and Recovery in Britain, 1914-1930, London 2010; Roper, Michael: The Secret Battle. Emotional Survival in the Great War, Manchester 2009.
- ↑ Winter, Jay: Shell Shock and the Cultural History of the Great War, in: Journal of Contemporary History 35/1 (2000), pp. 7-11; Acton, Carol and Potter, Jane: These frightful sights would work havoc with one’s brain: Subjective Experience, Trauma, and Resilience in First World War Writings by Medical Personnel, in: Literature and Medicine 30/1 (2012), pp. 61-85.
- ↑ Lerner, Paul: Hysterical Men. War, Psychiatry and the Politics of Trauma in Germany, 1890-1930, London et al. 2003, p. 2.
- ↑ Crouthamel, Jason: The Great War and German Memory. Society, Politics and Psychological Trauma, 1914-1945, Exeter 2009.
- ↑ Cited in: Becker, Annette: Guerre Totale et Troubles Mentaux, in: Annales. Histoire, Sciences sociales 55/1 (2000), pp. 135-152.
- ↑ Thomas, Gregory M.: Treating the Trauma of the Great War. Soldiers, Civilians, and Psychiatry in France, 1914-1940, Baton Rouge 2009. For the "intellectual confusion" surrounding debates about the First World War see Audoin-Rouzeau, Stéphane and Becker, Annette: 14-18: Understanding the Great War, New York 2000, pp. 1-12.
- ↑ van Bergen, Leo: Before My Helpless Sight. Suffering, Dying and Military Medicine on the Western Front, 1914-1918, Farnham et al. 2009; Harrison, The Medical War 2011; Binneveld, Hans: From Shell Shock to Combat Stress. A Comparative History of Military Psychiatry, Amsterdam 1997; Harrison, Mark / Cooter, Roger / Sturdy, Steve: War, Medicine and Modernity, Stroud 1998.
- ↑ Harrison, The Medical War 2011, p. 261.
- ↑ Kaes, Anton: Shell Shock Cinema. Weimar Culture and the Wounds of War, Princeton et al. 2011, p. 39; Hofer, Hans-Georg and Prüll, Cay-Rüdiger: Reassessing War, Trauma, and Medicine in Germany and Central Europe (1914-1939), in: Hofer/Prüll/Eckart, War, Trauma and Medicine in Germany 2011, p. 18.
- ↑ Thomas, Treating the Trauma of the Great War 2009, p. 25.
- ↑ For example see Mercier, Charles: Science and Education, in: The Times, 17 January 1916, p. 9.
- ↑ Elliot Smith, Grafton and Hatherley Pear, Tom: Shell Shock and its Lessons, Manchester 1917, Preface.
- ↑ Myers, Charles: A Contribution to the Study of Shell Shock, in: The Lancet, 13 February 1915, pp. 316-320.
- ↑ For Wilfred Owen's Mental Cases and other war poetry see http://www.oucs.ox.ac.uk/ww1lit/collections (retrieved: 28 February 2013); W.L.: Kaye, Henry Waynard, Unpublished War Diary, 5 March 1916.
- ↑ Winter, Shell Shock and the Cultural History 2000, pp. 9-10.
- ↑ For a full discussion of diagnostic inconsistencies among French doctors see Thomas, Treating the Trauma of the Great War 2009, pp. 51-61.
- ↑ Salmon, The Care and Treatment of Mental Diseases 1917, p. 517.
- ↑ Lerner, Paul and Micale, Mark: Trauma, Psychiatry and History. A Conceptual and Historiographical Introduction, in: Micale and Lerner (eds.), Traumatic Pasts 2001, p. 6.
- ↑ Jones and Wessely, Shell Shock to PTSD 2005, p. 14.
- ↑ Micale, Mark: Hysterical Men. The Hidden History of Male Nervous Illness, Cambridge, Massachusetts et al. 2008, p. 130.
- ↑ Ibid., p. 194.
- ↑ Showalter, Elaine: The Female Malady. Women, Madness and English Culture, 1830-1980, London 1987.
- ↑ Lerner, Hysterical Men 2003, pp. 6-7.
- ↑ Young, Allan: The Harmony of Illusions. Inventing Post-Traumatic Stress Disorder, Princeton 1995, pp. 61-62.
- ↑ Notice from the War Office, in: The Lancet, 31 July 1915, p. 261.
- ↑ Prüll, Cay-Rüdiger: ‘The Exhausted Nation-Psychiatry and Medicine on the Home Front (1914-1919). The Case of Robert Sommer and the City of Giessen in: Hofer/Prüll/Eckart, War, Trauma and Medicine in Germany 2011, p.43.
- ↑ Bianchi, Bruna: Psychiatrists, Soldiers, and Officers in Italy during the Great War, in: Micale and Lerner (eds.), Traumatic Pasts 2001, p. 231.
- ↑ Lerner, Hysterical Men 2003, p. 33.
- ↑ Thomas, Treating the Trauma of the Great War 2009, pp. 33-35.
- ↑ Myers, Charles: Shell Shock in France, 1914-1918, Cambridge 1940, pp. 102-107.
- ↑ Salmon, The Care and Treatment of Mental Diseases 1917, p. 521.
- ↑ Lerner, Hysterical Men 2003, p. 57.
- ↑ Hofer, Hans-Georg: Beyond Freud in: Hofer/Prüll/Eckart, War, Trauma and Medicine in Germany 2011, pp. 49-71.
- ↑ W.L. PP/CMW/I3/1. Moran, Charles: Handwritten notes for book on shell shock (undated).
- ↑ Moran, Charles: The Anatomy of Courage, Cambridge 1945, p. x.
- ↑ Smith, Leonard V.: The Embattled Self. French Soldiers’ Testimony of the Great War, Ithaca 2007, p. 32.
- ↑ Best, Geoffrey: Humanity in Warfare, London 1980. The best example of pacifists accepting military work is the Friends’ Ambulance Unit. See Brown, Michael: The Evolution of the Friends’ Ambulance Unit, London 1943.
- ↑ Mott, Frederick, The Lettsomian Lecture, in: The Lancet, 11 March 1916, p. 549.
- ↑ Miller, Emanuel (ed.): The Neuroses in War, London 1940, p. 124; Peckl, Petra: What the Patient Records Reveal: Reassessing the Treatment of “War Neurotics” in Germany (1914-1918), in: Hofer/Prüll/Eckart, War, Trauma and Medicine in Germany 2011, p. 139.
- ↑ For documentary footage of men being treated at Seale Hayne see http://www.britishpathe.com/workspaces/BritishPathe/shell-shock (retrieved: 28 February 2013).
- ↑ Hurst, Twentieth Century Physician 1949, p. 168.
- ↑ http://www.sciencemuseum.org.uk/broughttolife/people/williamrivers.aspx (retrieved: 28 February 2013); Shephard, Ben: The Early Treatment of Mental Disorders, in: Berrios, Hugh and Freeman, Lionel (eds): 150 Years of British Psychiatry, London 1996, pp. 434-464 (p. 444).
- ↑ Lerner, Hysterical Men 2003, p. 89; Thomas, Treating the Trauma of the Great War 2009, p. 39.
- ↑ Ash, Edwin: Letter to The Lancet, 27 January 1917, pp. 165-6.
- ↑ Yealland, Lewis: Hysterical Disorders of Warfare, London 1918; Miller, Emmanuel (ed.): The Neuroses in War, London 1940, p. 123.
- ↑ Roudebush, Marc: A Patient Fights Back: Neurology in the Court of Public Opinion in France during the First World War, in: Journal of Contemporary History 35/1 (2000), pp. 29-38.
- ↑ W.L. RAMC 446/18.Kirkwood, G.N., 9 July 1916.
- ↑ Lerner, Hysterical Men 2003, pp. 228-29.
- ↑ For veterans’ sarcastic use of the phrase see Crouthamel, Jason: War Neurosis versus Savings Psychosis: Working Class Politics and Psychological Trauma in Weimar Germany, in: Journal of Contemporary History 37/2 (2002), p. 174.
- ↑ Reid, Broken Men 2010, p. 144.
- ↑ Lerner, Hysterical Men 2003, p. 228.
- ↑ Crouthamel, War Neurosis 2002, p. 173.
- ↑ Thomas, Treating the Trauma of the Great War 2009, pp. 125-126.
- ↑ Ibid., pp. 134-136.
- ↑ Orwell, George: Down and Out in Paris and London, London 1984, p. 140. [First published London 1933.]
- ↑ For an overview of high and low culture in the Weimar republic see http://www.germanhistorydocs.ghi-dc.org/sub_imgs.cfm?section_id=12 (retrieved 28 February 2013) for Otto Dix see http://www.ottodix.org (retrieved 28 February 2013) for Otto Dix and George Grosz see collections at MoMA: http://www.moma.org/collection/artist.php?artist_id=1559 (retrieved 28 February 2013); http://www.moma.org/collection/artist.php?artist_id=2374 (retrieved 28 February 2013); Becker, Annette: The Avant-Garde, Madness and the Great War, in: Journal of Contemporary History 35/1 (2000), pp. 227-56.
- ↑ ESWS is now known as Combat Stress. See http://www.combatstress.org.uk/ (retrieved 28 February 2013); National Archives WO/32/4742, Lord Southborough, House of Lords, 28 April 1920.
- ↑ HMSO Report of the War Office Committee of Enquiry into Shell Shock, London 1922, pp. 122-23.
- ↑ Miller, The Neuroses in War 1940, p. 127.
- ↑ Wessely, Simon: The Life and Death of Private Harry Farr, in: Journal of the Royal Society of Medicine 99 (September 2006), pp. 440-443. See http://www.rsm.ac.uk/media/pr212.php (retrieved 28 February 2013).
- ↑ Smith, The Embattled Self 2007, p. 159.
- ↑ Herbert, Alan: The Secret Battle, London 1919; Churchill, W.S.: Preface to: Herbert, Secret Battle, London 1928.
- ↑ Hofer, Beyond Freud 2011, pp. 62-64.
- ↑ Bourke, Joanna: Effeminacy, Ethnicity and the End of Trauma: the Sufferings of “Shell Shocked” Men in Great Britain and Ireland, 1914-1939, in: Journal of Contemporary History 35/1 (2000), pp. 60-62; Thomas, Treating the Trauma of the Great War 2009, pp. 64-65.
- ↑ Standwell, T.W.: Are You a Potential Post-War Criminal?, in: Health and Strength (24 January 1920), p. 62.
- ↑ For a full account see Crouthamel, The Great War and German Memory 2009, especially Chapter 3.
- ↑ Crouthamel, War Neurosis 2002, p. 177.
- ↑ Ibid., p. 178.
- ↑ Crouthamel, The Nation’s Leading Whiner 2011, p. 83.
Selected Bibliography
- Barham, Peter: Forgotten lunatics of the Great War, New Haven 2004: Yale University Press.
- Crouthamel, Jason: The Great War and German memory. Society, politics and psychological trauma, 1914-1945, Exeter 2009: University of Exeter Press.
- Harrison, Mark: The medical war. British military medicine in the First World War, Oxford; New York 2010: Oxford University Press.
- Hofer, Hans-Georg / Prüll, Cay-Rüdiger / Eckart, Wolfgang Uwe (eds.): War, trauma and medicine in Germany and Central Europe, 1914-1939, Freiburg 2011: Centaurus Verlg.
- Jones, Edgar / Wessely, Simon: Shell shock to PTSD. Military psychiatry from 1900 to the Gulf War, Maudsley monographs, number 47, Hove; New York 2005: Psychology Press.
- Kaes, Anton: Shell shock cinema. Weimar culture and the wounds of war, Princeton 2011: Princeton University Press.
- Leed, Eric J.: No man's land. Combat & identity in World War I, Cambridge; New York 1979: Cambridge University Press.
- Lerner, Paul Frederick: Hysterical men. War, psychiatry, and the politics of trauma in Germany, 1890-1930, Ithaca 2003: Cornell University Press.
- Reid, Fiona: Broken men. Shell shock, treatment and recovery in Britain, 1914-1930, London; New York 2011: Continuum.
- Roper, Michael: The secret battle. Emotional survival in the Great War, Manchester; New York 2009: Manchester University Press.
- Shephard, Ben: A war of nerves. Soldiers and psychiatrists, 1914-1994, London 2002: Pimlico.
- Thomas, Gregory Mathew: Treating the trauma of the Great War. Soldiers, civilians, and psychiatry in France, 1914-1940, Baton Rouge 2009: Louisiana State University Press.
- Van Bergen, Leo: Before my helpless sight. Suffering, dying and military medicine on the Western Front, 1914-1918, Farnham; Burlington 2009: Ashgate.