Introduction↑
In the past decades, historians have increasingly treated the theme of “disease in the First World War” by highlighting medicine and technology, the social and cultural effects of disease, as well as the national and international politics of public health. Some studies have investigated the spread of disease during the First World War through the lens of biological manifestations of illness and the related medical and technological capacity to respond.[1] Historians have explored the social and cultural effects of disease, as well as the place of “the sick,” whether soldiers or civilians, in the realm of policymaking.[2] Examples of this are studies that have looked at the nexus between health, disease, nation-building and state-building during and after the war.[3] Furthermore, there has been recent attention given to health and disease as objects of international governance via institutional networks of relief and rehabilitation.[4]
This article integrates the extant literature in an overview of disease diffusion during the war, its exogenous causes, as well as state and non-state responses to sickness during and immediately after the conflict. By looking primarily at epidemic crises, this analysis first explores wartime conditions and the extent of human and material destruction. It moves out from this to view the response shown in state efforts, private initiatives, external humanitarian aid, as well as the international governance of health in the post-war. National and international responses to disease at the time were deeply entwined with post-war politics, diplomatic relations, or economic agendas. This article focuses primarily on planning, intended methods, and the practice of relief. Chronologically, the article treats the topic from the early days of the war until its aftermath. In including the post-war period, this overview draws attention to the fluidity and pervasive effects of disease after the formal end of the conflict, as well as to the way it shaped the making of post-war internationalism.
Disease in Times of War↑
In 1914, the Austro-Hungarian Empire invaded Serbia. The First World War started formally and weeks of battle followed in this small country, resulting in casualties among soldiers and civilians. Lice and typhus, already causing havoc among the military of Austria-Hungary, spread quickly in Serbian territory, infecting and eventually killing civilians. The typhus epidemic was just one of many health crises caused by infectious diseases during the First World War. Bacterial, viral or parasite-based diseases such as malaria, dysentery, cholera, typhoid, tuberculosis, smallpox, and venereal diseases killed more people than military clashes, and weakened armies and entire societies during the four years of combat. Further, by 1918, the influenza pandemic crippled theaters of war, as well as neutral territories in and beyond Europe.
The First World War saw entire armies decimated; soldiers were injured in battle or physically affected by disease. Famine emerged and quickly deepened, and civilians were uprooted and forced to find new homes. Inevitably, the health of both soldiers at the front and those left at home took a dramatic turn; physical destruction, hunger, poverty, soldiers’ constant mobility and non-combatants’ forced displacement determined an environment that supported the development of diseases and other, often interrelated, health crises such as malnutrition. The following section offers an overview of the demographic dimensions of disease-driven destruction and explores its causes.
Wartime Conditions↑
The context of the First World War created conditions that enabled the fast spread of various viral and bacterial infections. A direct connection between the First World War and the sudden emergence of epidemics remains diffuse. Some diseases (e.g. typhus, cholera) had been endemic prior to the war. However, wartime events and conditions – a poor material infrastructure, a lack of medical capacity to address epidemics, crises in food supplies, the soldiers’ and civilians’ dual state of confinement and mobility – weakened immune systems and hampered people’s immediate care.
The lack of proper medical care worsened the situation in most regions. All belligerents were largely unprepared for a long war and medical forces were simply not enough to address the effects of disease from the early days of the conflict.[5] In France, medical personnel and vehicles were lacking at the height of a tuberculosis crisis, despite a significantly stronger logistical capacity than other countries.[6] In the early days of war, in 1914, the Austro-Hungarian Empire had a critical shortage of doctors; the army entered the war with 1,400 doctors and only 191 military hospitals with 17,709 beds.[7] In Serbia, Poland or Romania, there were not enough hospitals for isolating or even sheltering soldiers or civilians, and there were too few doctors and nurses. A British doctor deployed to Serbia claimed that in a military hospital where he was performing surgical duties there were at one time 1,600 sufferers, more than 1,000 of them diagnosed with typhus; and this in a hospital that in peace time had had beds for 400 patients.[8]
Poor living conditions as a result of insufficient material infrastructure became clear when infectious diseases spread. The causes often lay in a substandard transportation infrastructure, inadequate clothing especially for troops, little proper access to clean water, and an absence of general sanitary conditions. Typhus, dysentery, tuberculosis or malaria had ideal breeding grounds in conditions of overcrowded and dirty bodies. Limited access to hygiene coupled with environmental conditions worsened the intensity of disease, as both winters and summers enabled the transmission of parasites or viruses. A hot climate, for example, generated the fast spread of dysentery within the German military[9] and of malaria in Southern Italy and in the Ottoman Empire.[10]
The food crises in various theaters of war decreased the human body’s capacity to fight infections. Events such as the German army’s invasions in the East or the Allies’ blockade of Germany caused crises of hunger, leading to a worsening in the health of many civilians. In Germany, from 1915 onwards, food shortages and inflated prices meant limited access to resources for a large proportion of the population at home. A harvest failure in 1916 contributed to food crises, with a significant impact on people’s bodies. Inadequate food supplies and a lack of proper nutrition affected children’s growth, as well as their stamina and immune systems. It was among older people that the unsatisfactory level of nutrition had the most serious consequences; their resistance to disease plummeted and acute illness affected them quickly and severely. Tuberculosis, in particular, was increasingly present among urban dwellers, who lived closer together and felt food shortages more than civilians based in rural areas.[11] At the time of the food crisis in Germany, on the Eastern Front, the Central Powers’ invasions led to looting and the subsequent takeover of foodstuff and infrastructure supplies. Civilians were left without access to food, and starvation raised public health concerns.[12]
Troops also suffered from malnourishment. Austro-Hungarian soldiers frequently lamented the lack of proper nutrition,[13] while the 3rd Army of the Ottoman Empire suffered from aggressive epidemics attributable to a lack of food supplies among the military at the front.[14] In these conditions of malnutrition, tuberculosis, malaria, typhoid or cholera, diseases associated with an inadequate digestive system, were prevalent.
The wartime refugee crisis also generated a favorable environment for infections to multiply. Often moving on foot, with a limited amount of food or clothing, without medical care or access to clean water and proper hygiene, many refugees fell ill and even lost their lives when in transit.[15] In one case, internal displacement in Russia saw overcrowding in villages, towns and cities. Historian Peter Gatrell describes the state of health as “heart-rending” in terms of refugee mortality in Turkestan where children, in particular, suffered from epidemics of smallpox and typhus, and where hot summers threatened an outbreak of malaria.[16] In Austria-Hungary, people of the empire’s borderlands, evacuated by the army, were placed in approximately thirty refugee camps. The Ministry of Internal Affairs first claimed that these placements were to control the evacuees, especially from a sanitary point of view.[17] Despite these claims, the struggling central institutions of Austria-Hungary offered a poor response to the spread of various epidemics and these camps initially lacked proper access to hygiene and palliative care. The overcrowding in these spaces of confinement led to a severe deterioration in the health of these displaced civilians. Typhus fever was particularly widespread, with mortality rates rising to 29 percent in the camp at Thalerhof, in southeast Austria. In addition to typhus, dysentery, cholera, measles or scarlet fever led to a particularly high infant mortality rate in these refugee camps.[18]
Confinement exacerbated the spread of infectious diseases among soldiers as well. Prisoners of war (POW) camps were breeding spaces for infection. Reports of German and Austro-Hungarian POWs interned on the Eastern Front note that poor and limited nutrition caused illnesses related to the digestive system, especially dysentery.[19] Typhus broke out in Germany and Russia in 1915. Overcrowding, as well as difficult climate conditions and a lack of access to water during winter in Siberian camps affected the health of POWs. In one instance, it was reported that in Russia at Totskoe camp, 10,000 men died of typhus.[20]
Besides overall wartime devastation, displacement, poor infrastructure or medical care, troops’ constant mobility arguably generated the fast spreading of various microbes, parasites or viruses. This was certainly the case of the typhus that was rife among the soldiers of Austria-Hungary and which spread in Serbia once they invaded in 1914. Worst of all, however, was the emergence of influenza and its immediate spread once combatants returned home at the end of the war.
A plethora of analyses have come out over the past century, all trying to understand the connection between the war itself and the emergence and extent of the 1918-1919 influenza pandemic. Nonetheless, in general, there is no consensus regarding the origin of the disease. The conventional argument points to two big military camps in the US (Camp Funston, Fort Ripley and Camp Oglethorpe, Georgia) and the American soldiers’ movement into continental Europe in 1917 as causes of the rapid spread of the virus among troops and civilians in the epicenters of the conflagration.[21] Other arguments place the origin of the virus in China, in the winter of 1917-1918, or in France in 1916.[22]
The transformation of a local epidemic into a pandemic lay at the heart of the global nature of the war, which involved battlefields beyond Europe, including in Asia and Africa, and various imperial subjects called to defend the interests of governments.[23] Various populations came into contact with one another and, as soon as the war ended, many combatants returned home by steam ship and traveled on to their homes. In New Zealand and Japan, there was a belief that the virus arrived by naval ships anchored in these countries’ ports.[24] In India, the pandemic arguably originated from troops returning home and passing on the disease to civilian populations, as they traveled by train into the interior of the country.[25] Similarly, in South Africa, one of the worst hit regions, two troopships from England carrying black South African Labour Corps soldiers arrived in Cape Town, after a stopover in Freetown, Sierra Leone, where the influenza was already rife.[26] Besides this repatriation-oriented mobility, it is important to consider the ways wartime conditions generated other types of crises that, arguably, affected the extent of the influenza pandemic. After four years of combat, belligerent countries suffered from a lack of medical human resources, already limited in capacity and increasingly crippled by the various health crises during the war, diminished economies, the growth of poverty among civilian populations, or limited access to palliative care; all these factors, induced by the war, contributed to the spread of the influenza in the immediate aftermath of the conflict.
The Sick and the Dead: A Few Numbers↑
From the armistice onwards, historians, demographers, and statisticians have agreed that disease generated grave suffering and a significant proportion of casualties.[27] Generally, it is difficult to properly quantify the extent and effects of disease on soldiers and civilians. First, when it comes to infections, certain epidemics affected some regions and population sections more than others. Second, there is more information about soldiers’ health and their mortality rates caused by disease than civilian cases, largely because of the organized nature of the military and its medical care. Lastly, there is significant heterogeneity in terms of regional availability of data, as Western European states have provided more statistics and demographic patterns. Taking this into account, this subsection uses some key studies and maps the main epidemiological crises and the extent of the devastation that disease caused.
When it comes to combatant losses of the British Empire, various data was reported in the decades after the war. One report on statistics around military losses of the British Expeditionary Forces claimed that a total of 111,073 combatants (out of 880,000 total victims) perished from injury and illness; still, there is no information regarding specific diseases and their effects on mortality rates.[28]
Historian Jay Winter revisited civilian health in Great Britain during the Great War, from a demographic perspective. Winter pointed to 1915 as a year of high mortality due to influenza, bronchitis, or pneumonia; further, the study included common diseases of childhood, such as whooping cough, diphtheria, and measles, as well as tuberculosis and meningitis.[29]
In the case of France, statistician Michel Huber showed that mortality rates caused by disease among the population doubled between 1914-1918, when compared to the pre-war period. For instance, the typhoid fever rate in 1913 was of 3,600 noncombatants, whereas in 1914 it rose to 8,700. Diphtheria caused an increase in deaths from 2,300 in 1914 to 4,200 in 1918.[30] Furthermore, tuberculosis generated a high rate of sickness and related deaths in France. The existing numbers of civilian casualties point to a high mortality rate: 64,200 civilian deaths were registered in 1914 alone. Tuberculosis was the most prevalent epidemic among French soldiers. According to data of the Military Health Service, from August 1914 until June 1919, 150,000 cases of tuberculosis were detected and approximately 40,000 soldiers died in boot camps and in the army.[31]
In Italy, various statisticians collected information in the 1920s and claimed that the sick amounted to an estimated number of 2,500,999.[32] The rates of hospitalization peaked in 1915 after new cases of cholera appeared, four years after the seeming eradication of the 1910-1911 wave in the southern part of the country.[33] A second peak came in 1918, due to the influenza crisis. Malaria caused further havoc with 120,000 registered cases. One study notes that in the province of Puglia, in southern Italy, in 1918 there were more deaths than in the entire country in 1914.[34] Approximately 130,000 people fell ill of typhoid, tuberculosis, cholera (including 5,000 deaths) or measles.[35]
The Central Powers also battled high degrees of sickness and related losses among civilians and the military. In the case of Germany, an overall view of the medical state of soldiers suggests that infectious disease led to high morbidity and mortality among army men. For example, a 1934 sanitary report provided by the German state, pointed to almost 2 million army casualties (including illness and injury).[36] Doctors notably treated more than 19 million cases of disease, including civilians, among which infections totaled only approximately 2 million instances.[37] The second half of the war saw a growth in civilian morbidity caused by disease, a statistic suggested by the high number of male civilian deaths in 1919 when compared to 1914. It is most probable that many of these men were returned soldiers and that service had had an impact on their health. Among women, casualties of tuberculosis rose to over two-thirds from 1914 to 1918. Deaths caused by pneumonia, a disease that indicated poor social conditions, more than doubled from 1914 to 1918.[38]
A recent statistical publication regarding the experience of war in the Austro-Hungarian Empire showed that the army struggled with typhus, typhoid fever, smallpox, cholera or dysentery. Epidemics affected a total of 3,188,000 people in the military personnel between 1914 and 1918. Further, according to this report, various lung infections and influenza led to the death of approximately 697,994 people during the war in the Austrian part of the empire. In wartime Hungary, 2,164,708 people died from the same afflictions between 1914-1918. [39]
In the Ottoman Empire, reports of lack of supplies and rampant epidemics are mirrored in data estimated subsequently. For instance, a medical report claimed that the total number of military casualties of the Ottoman army was 771,844, with illnesses resulting in 466,759 casualties.[40] Turkish historian Hikmet Özdemir totaled data from the Army Medical Department and suggested that 330,796 army casualties were caused by disease, primarily dysentery (40,000), typhus (26,000), malaria (23,351), recurrent fever (4,000), or syphilis (150).[41] In both calculations, almost half of Ottoman soldiers died because of health problems.
In contrast to some of the specifics regarding deaths by disease in Austria-Hungary or the Ottoman Empire, data regarding the Russian Empire remains unclear. A publication financed by Carnegie Endowment for International Peace wrote that by the end of March 1914, 13 million men were fighting in the army and over 4.8 million fell ill, mostly from infections. The study further argues that the entire population of the Russian Empire fell by 6 million by the end of 1917.[42] Still, little is known about the specifics of various diseases and their effects on casualties in Russia. Arguably, the high rate of forced displacement and the lack of detailed data regarding the army structure render these statistics incomplete.
Similarly, in the case of Eastern Europe, little is known about the total of disease-related casualties and direct demographic effects of sickness among combatants and civilians during the war. Arguably, this can be attached to the poor institutional centralization of public health, as well as to the sociopolitical changes that this region went through after the Paris Peace Conference. The case of Romania is indicative; a Ministry of Health was established as late as 1923 and the first large population census took place in 1930.[43]
The above outline of numbers and related diseases highlight various epidemiological crises that caused significant damage, in different degrees, among soldiers and civilians. It was, however, the “Spanish flu”, or the influenza pandemic, that affected all parts of the world, not only those close to warzones. Indeed, the pandemic infected about 500 million people (one-third of the world’s population) and caused the deaths of approximately 50 million people all over the world. An in-depth analysis of the casualties and infection rates caused by the influenza pandemic is beyond the immediate purposes of this article. Various historians have already compiled the existing and often detailed data regarding the infection rate and numbers of casualties. These studies range from regional and country-focused to macro-approaches that mark worldwide trends. Still, similarly to the case of the aforementioned epidemiological crises, data remains sparse and largely heterogeneous. Nonetheless, various estimates show that the highest death rates were in Sub-Saharan Africa, South and East Asia, Central America, and the Pacific Islands; at the same time, North America and Europe, conventionally considered the origins of the pandemic, had lower mortality rates caused by influenza.[44]
Domestic Responses to Disease↑
Once disease claimed significant numbers of victims in national armies and among civilians, state institutions responded with curative, as well as preventive, measures. Most state resources went into providing armies with enough material and human infrastructure to address infections among soldiers and avoid the practical weakening of fighting forces during the war. State and local officials addressed the civilian plight as well, but various private initiatives mobilized, primarily to help the vulnerable members of society: women, children, and the elderly.
State Efforts↑
First, there was support given to the medical infrastructure with the purpose of assisting sick soldiers, once it became clear that the war would not be as short as predicted. In France, the army entered the war with 191 military hospitals, but by the end of 1916 it had acquired 133 medical and sixty surgical trains, 266 field hospitals, 200 mobile surgical groups, 300 permanent hospitals for epidemic disease, and it established 151 bacteriological laboratories.[45] The British Royal Army Medical Service started the war with 1,000 doctors and nurses, but by 1918 there were over 160,000 doctors and nurses.[46] By 1918, the understaffed Austro-Hungarian medical military increased the number of hospitals to 874, with 95,000 beds.[47] The Ottoman government also increased the number of hospitals and used pre-existing health institutions to assist the army. The Ottoman military further organized mobile hospitals near the fronts.[48]
The military personnel in and around warzones engaged with palliative care in the hospitals of the battlefield, coupled with preventive vaccination and disinfection. British military doctors in particular focused on implementing strict rules of hygiene and vaccination. Historian Mark Harrison has argued that within two years British vaccination rates of men in uniform had risen above 90 percent, with undeniable positive results. The proportion of British soldiers contracting typhoid fever dropped, as seen in hospital admission rates: from a peak of 3.1 admissions per 1,000 troops in 1915 to 0.2 in 1918.[49] By contrast, German military authorities focused on aggressive disinfection, with hygienists implementing strong rules among the army corps. Still, this approach had mixed results. If cholera or typhoid were largely kept at bay, dysentery became rife due to lack of vaccines early in the war and to still-defective hygiene education.[50]
Palliative measures were designed to contain epidemic outbreaks. However, in some cases, prevention was also part of health policy towards soldiers on the battlefield. For example, Nic Clarke and his co-authors highlight that the organization of combat had positive effects on Canadian soldiers’ health. Many of the young male soldiers had been recruited from lower-class urban backgrounds, crippled by poor nourishment, poor eyesight and dentition, and even suffering from musculoskeletal, neurological or psychiatric disorders. The overall management of Canadian troops included limited time in frontline trenches, care over nutrition and diet, as well as medical care for various physical disorders, which improved many soldiers’ fitness and overall health when fighting in the war.[51]
On the home fronts, domestic agencies and local authorities were effectively in charge of managing health crises among civilians. This was the case in Eastern Europe, for instance, where the lack of medical personnel and shortages in medication or technology (e.g. microscopes, sterilization) led to a preference for aggressive and highly intrusive disinfection measures. In Serbia, authorities fought typhus through decontamination of houses, trains and clothes. In the city of Belgrade, a Hygiene Commission was responsible for disinfection of public spaces and private apartments. Strict regulation governed the sanitary conditions of cafes and other public places (i.e. short opening times and daily disinfection with petroleum). For the army, military personnel used hot-air ovens and Sulphur fumigation.[52] In German-occupied Poland, Germans employed severe tactics for disinfecting the population, often forcing the closure of institutions and businesses deemed unclean. Those measure had inherent discriminatory undertones, as targeted individuals were often poor Jews, deemed incapable of maintaining basic hygiene. Beyond this, in April 1918, Poland established its own Ministry of Public Health, Social Welfare and Labor Protection. This Ministry planned a comprehensive scheme to fight the epidemic by establishing hospitals and cleaning stations on the borders, in order to avoid infections spreading from the East.[53] In contrast to the Serbian and Polish cases, the Ottoman authorities preferred more preventive measures. When typhus, dysentery, typhoid, cholera or malaria outbreaks were reported, health officials organized vaccination campaigns and hygiene education measures for both soldiers and non-combatants. Further, civilians were taught how to ward off lice, how to maintain water cleanliness, how to disinfect household items, and how to keep mosquitoes at bay.[54]
Quick logistical responses to prevent future epidemiological crises also showed improvement in civilian health. Jay Winter has suggested that this was the case in Great Britain, where a series of policies including the development of infrastructure capacity, support for growth in human resources, and targeted fundraising campaigns, improved infant and mother welfare, and alleviated child mortality rates during the war.[55]
After the peak of the influenza pandemic passed, various states committed to the spurring of policy initiatives to prevent a similar disaster. Attempts to create efficient public health systems through centralization of various health departments were measures implemented in Great Britain, Canada, Austria, and South Africa. Local administration of towns and regions sustained general supplementation in human resources and physical infrastructure in France, New Zealand, or India.[56]
Private Initiatives↑
While many efforts were undertaken by state institutions to address the health crises of both soldiers and civilians, it was the former that absorbed the bulk of finance and care. In this context, the fate of civilians was often left to various private charitable initiatives that developed wartime programmes to address the plight of the sick.
Generally, formal organizations of private aid were established and managed to address disease among civilians. These associations, organized primarily by women on the home front, focused on the relief of children, their mothers, as well as the elderly. In France, there was a boom in child-oriented charitable initiatives from the early days of the war. Among them, L’Orphelinat des Armées, put the health of children high on their agenda.[57] In Germany, the Kaiserin Auguste Viktoria Haus was involved in infant care.[58] Anitta Müller-Cohen (1890-1962), a twenty-four year old Jewish woman, organized food and medical relief in Vienna on behalf of children and mothers, as well as refugees arriving in the capital.[59] In Poland, Adam Sapieha’s (1867-1951) Relief Committee focused on childcare and it organized sanitary departments. In Hungary, the Stefania Association for the Protection of Mothers and Infants trained volunteers in healthcare and assisted child health.[60]
Other private initiatives had a communitarian basis and agenda. This was the case of Jewish organizations in Eastern Europe, whose work focused on relieving Jewish civilians. The belief that Jews were filthy and the unclean conditions in the Jewish districts of Polish cities fueled the idea that anti-typhus efforts in Poland should be targeted primarily towards these groups. The invasive and often brutal methods that targeted Jewish populations however were simply curative, with little attention given to prevention and living conditions. In this context, the Saint Petersburg based Society for the Protection of the Health of the Jewish Population (OZE) attempted to open new doctor’s surgeries, hospitals or sanitary supervision.[61] In another instance, Jewish-based relief in Romania followed a more general approach, where smaller initiatives of general hygiene measures, nursing or food relief shaped communitarian aid for Jewish children, women and the elderly.[62] Austrian Jews also mobilized financially to improve the quality of hospitals and paid for care of both soldiers and civilians within the Austro-Hungarian Empire.[63]
In terms of non-governmental assistance of those affected by the spread of disease, national Red Cross branches managed and directed private care. The Red Cross in France, Italy, Germany, Austria-Hungary, Romania, Poland, and Russia, as well as the Ottoman Red Crescent Society, were active during the hostilities. Often logistically supported by state institutions and drawing funds from charitable activities, Red Cross societies set up ad-hoc and often short-lived hospitals, sanitaria, or sanitary courses for both civilians and soldiers.[64]
External Humanitarianism for the Sick↑
Despite forms of state and private mobilization to address the various disease crises, the financial and logistical effects of the war curtailed the outreach and effectiveness of these domestic channels of assistance. In this context, state officials or representatives of various private initiatives sought external aid arriving via formal humanitarian efforts. During the war, various humanitarian organizations delivered aid to conflict-laden areas of Europe. These organizations were established during the war or specifically routed their activity towards war sufferers. In this context, alleviation of disease-driven suffering that had caused havoc among soldiers and civilians became one of the main rationales of emergency relief and transnational humanitarian practice.
National Red Cross societies went abroad to address health crises and implement curative and preventive medical assistance to alleviate the suffering among soldiers and civilians. For example, British Red Cross and Canadian Red Cross doctors and nurses traveled to Eastern Europe to support the medical infrastructure needed to combat infectious diseases such as typhus. The Austrian Red Cross, Swedish Red Cross or Danish Red Cross missions traveled to Russia with a POW relief effort sustained by a group of volunteer nurses.[65] Early on, in 1914, the Japanese Red Cross sent doctors and relief workers to Europe, in order to assist the military medical services of the Allied countries.[66]
The American Red Cross (ARC) became the national branch with the most extensive humanitarian activity abroad during the war. One-third of the population joined as members, $400 million were donated in 1917 and 1918 alone, and bankers and businessmen took charge of its institutional organization. This was strengthened by an impressive spirit of volunteerism as American physicians, social workers, nurses and other professionals crossed the Atlantic with the purpose of relieving war sufferers, including those hit by sickness. The ARC provided medical assistance, food, and clothing in and outside European battlefields. In fact, one of the first missions was to Serbia, to address the outbreak of typhus. In 1915 the ARC appointed a Sanitary Commission to control the epidemic, also financed by a $145,000 appropriation from the philanthropic Rockefeller Foundation (RF). The commission arrived in the spring of 1915 in Serbia and erected disinfection stations, dispensaries, and mobile sanitary trains in the region. The Sanitary Commission returned to the United States of America in early October once the epidemic subsided, but the ARC remained to organize a hospital for women and children and established other health-oriented relief operations for civilian populations. In the rest of Eastern Europe, the ARC managed missions across warzones, providing health care to those injured in combat, as well as to the victims of contagions, erecting hospitals for soldiers and civilians. In Western Europe, the ARC led campaigns against tuberculosis in France and Italy, where the disease had been endemic among soldiers and civilians.[67]
In the meantime, the International Committee of the Red Cross (ICRC) was involved mostly in aiding POWs and interned civilians. The ICRC brought in doctors and delivered medicine on an emergency basis. Further, in order to address the physical struggles of the POWs, the organization called for the repatriation of sick POWs through international agreements.[68]
International Health Governance in the Post-war Period↑
On 11 November 1918, the Armistice signed at Le Francport signaled the end of the First World War. Violence and conflict remained prevalent in Central and Eastern Europe, as regional wars (e.g. the 1919 war between Romania and Hungary), the Russian civil war or paramilitary violence continued.[69] At the same time, the great influenza epidemic was causing many more deaths worldwide than had combat in the First World War.
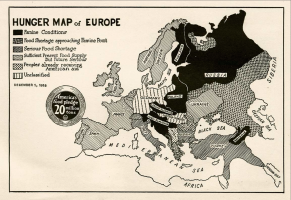
Outside the dramatic effects caused by influenza, western Europe saw a sharp decline in infectious diseases, as numbers had, for the most part, returned to pre-war levels by the 1920s.[70] However, further east, regions that continued to be plagued by violence and where domestic healthcare structures were underdeveloped, disease remained a substantial threat. In post-First World War and post-Civil War Russia in particular, famine was accompanied by cholera, dysentery, malaria, typhoid, typhus and relapsing fever. In Ukraine, a cholera epidemic broke out at the end of 1920 and again in 1921. In Poland, typhus reached epidemic proportions in 1919 and 1920.[71]
As infectious diseases continued to have devastating effects, humanitarian efforts on behalf of the sick continued, often in response to appeals for post-war aid. In June 1919, the ICRC set up the Central Bureau of a permanent international medical commission for the states that had been previously part of the Austro-Hungarian Empire and which were overrun by epidemics. The Bureau planned to organize a cordon sanitaire to stop epidemics from spreading, by setting up examination and disinfection centers on the borders. Further, in September 1919, the ICRC sent a fully equipped medical detachment to Ukraine, followed in June 1920 by a full medical mission composed of Swiss doctors and nurses.[72]
In the meantime, ARC’s post-war agenda focused on child health; related programmes were implemented in France, Italy, Greece and Eastern Europe. This work was largely rehabilitative, with a focus on prevention of disease. For this reason, hygiene, education, and nursing training took priority in the ARC’s post-war humanitarian efforts.[73] In 1919 the American-Jewish Joint Distribution Committee (JDC), established in 1914 to relieve Jews suffering in the war, arrived in Europe and brought in medical doctors, nurses, and medicines. In Poland, Romania, Slovakia, Lithuania or Latvia, JDC granted special funds to prevent and care for the many people suffering from typhus, smallpox, dysentery, or tuberculosis, which was common among Jews because of their poor living conditions. Restoring good sanitary conditions and supporting the infrastructure, as well as education, were among the JDC’s practices to relieve civilians in ill-health and reconstruct internal health structures in these regions.[74]
Besides supporting medical capacity and care, humanitarian organizations also focused on hunger relief as a way to alleviate the spread and impact of illnesses. The widespread food shortages and financial chaos of the war had generated hunger crises. In this context, leadership and volunteers attached to humanitarian organizations believed that malnourished children and starving adults would have impaired immune systems. Humanitarians therefore followed strict nutritional calculations and believed that proper quantities of food would fight and prevent infectious diseases. Fats, milk, sugar, cocoa, flour, peas, beans, or rice were distributed across Europe, in hospitals, as well as in schools or kindergartens.[75] For instance, in 1919, Herbert Hoover’s (1874-1964) European Children’s Fund, in collaboration with Clemens von Pirquet (1874-1929), the head of the Children’s Clinic in Vienna, developed a programme designed to provide foods of approximately 750 calories – containing fats, sugar, rice and cocoa – to European children. British and American Quakers and Save the Children, founded in 1919, also used food aid as the main source of relief and institutionalized large-scale programmes of child feeding.[76] However, these humanitarian endeavors were designed to be short-term, and focused on the whole on post-war emergency relief. By 1920, aid institutions looked at more long-term approaches in supporting the crippled post-war healthcare infrastructure, in order to prevent other epidemiological disasters.
Under the umbrella of “prevention” lay the activity of the American philanthropic organization the Rockefeller Foundation (RF). Besides the occasional support of the ARC in emergency relief for sick soldiers and civilians, the RF preferred long-term and reconstructive programmes. Once the war ended, the organization started assisting health and hygiene institutions across Europe; it funded research and experts, and sustained the development of rural infrastructure in various Eastern European states in the post-Armistice period.[77] Further, the RF also financially assisted the establishment and activities of the League of Nations Health Organization (LNHO).
In 1919, Jane Addams (1860-1935), a wartime worker on behalf of the US Food Administration and the first president of the Women’s International League for Peace and Freedom (WILPF), projected the idea that humanitarian aid, including relief work focused on health, should be a mechanism of international cooperation and should develop under the aegis of the League of Nations.[78] This international organization did not, however, assume the role of a humanitarian agent to alleviate the effects of health crises by means of food relief; it was, instead, a bureaucratic structure engineered to enable post-war health governance by means of international expertise via the LNHO. The genesis and the work of the LNHO placed the incidence of wartime disease at the heart of post-war internationalism. This institution aimed to engage state officials and health experts in order to address the effects of wartime illnesses and prevent new social disasters. The LNHO was born as a result of the leaders of states acknowledging their incapacity to address public health crises during the war. Thus, under the umbrella of the LNHO, various experts attempted to understand disease, epidemiological profiles and technical solutions. This agenda was evident early on, as the LNHO began collecting what historian Iris Borowy called “epidemiological intelligence” in Eastern Europe, starting with the still prevalent typhus.[79] Ultimately, the LNHO was an institutional form of transnational collaboration between state officials, health officers, practitioners and scientists. Its establishment followed an internationalist approach to health governance in the aftermath of the First World War.
Conclusion↑
The fight against the fast-spreading power of infections became what French reformer Georges Cahen (1875-1963) poignantly called “the other war.” The demographic disaster that various infectious diseases provoked during the First World War gives pertinence to Cahen’s description. Wartime conditions led to the emergence of illnesses that had been eradicated, or worsened the extent and effects of others. Disease affected the fighting capacity of armies, it shook states’ ability to respond in timely and potent ways, and fractured communities and entire societies. Military officials, state and local authorities, or health practitioners often struggled to contain epidemics. They were understaffed, lacking the financial, medical or technological means to address rampant sickness among soldiers and civilians. Still, the incidence of disease also played a significant role in the formation of states’ public health management and related reforms to cure and prevent physical decay. Further, it generated a mobilization of national and international civil society that claimed agendas of relief and rehabilitation of both combatants and civilians. Lastly, the wartime prevalence of disease and institutional capacity to respond during the conflagration created a salient backdrop for the making of post-war internationalism in health governance.
Doina Anca Cretu, European University Institute
Reviewed by external referees on behalf of the General Editors
Notes
- ↑ On role of doctors and technical capacity see for example Harrison, Mark: The Medical War. British Military Medicine in the First World War, Oxford 2010; Michl, Susanne: Im Dienste des “Volkskörpers:” Deutsche und französische Ärzte im Ersten Weltkrieg, Göttingen 2011; the collection of articles in Eckart, Wolfgang U./Gradmann, Christoph (eds.): Die Medizin und Der Erste Weltkrieg, Herbolzheim 2003.
- ↑ See the relationship between disease eradication, antisemitism and discrimination of Eastern Europeans in Weindling,Paul: Epidemics and Genocide in Eastern Europe,1890-1945, Oxford 2000; on public health in urban centers see Rollet, Catherine: The ‘Other War’ I. Protecting Public Health, in: Winter, Jay/Robert, Jean-Louis (eds.): Capital Cities at War. Paris, London, Berlin 1914-1919, Cambridge 1997, p.421-455.
- ↑ On public health in nation- and state-building and related responses to disease during and immediately after the war see for instance Kind-Kovacs,Friederike/ Bernasconi, Sara/Karge, Heike (eds.): From the Midwife’s Bag to the Patient’s File. Public Health in Eastern Europe, Budapest 2017; Turda, Marius/Weindling,Paul (eds.): Eugenics and Racial Nationalism in Central and Eastern Europe 1900-1940, Budapest 2007; Promitzer,Christian/ Trubeta,Sevasti/ Turda, Marius (eds.): Health, Hygiene and Eugenics in Southeastern Europe to 1945, Budapest 2011.
- ↑ Borowy, Iris: Coming to Terms with World Health: The League of Nations Health Organisation 1921-1946, Frankfurt am Main 2009; on imperial power and public health during the war see Winter, Jay: Military Fitness and Civilian Health in Britain during the First World War, in: Journal of Contemporary History Vol.15 (1980), pp. 211-244; for a recent analysis of the intersection between national and international governance of health see Silverstein, Sara: The Periphery is the Centre: Some Macedonian Origins of Social Medicine and Internationalism, in: Contemporary European History 28/2: Making Modern Social Science: The Global Imagination in East Central and Southeastern Europe after Versailles (2019), pp. 220-233.
- ↑ Herwig, Holger H: The First World War. Germany and Austria-Hungary, 1914-1918, London 2014, pp. 295-298.
- ↑ Murard/Zylberman, The Nation 2003, pp. 343-364.
- ↑ Herwig, The First World War 2014, p. 299.
- ↑ Soubbotitch,V: A Pandemic of Typhus in Serbia in 1914-1915, in: Proceedings of the Royal Society of Medicine, 11 (1918), p. 33.
- ↑ Linton, Derek: “War Dysentery” and the Limitations of German Military Hygiene during World War I, in: Bulletin of the History of Medicine, 84/4 (Winter 2010), pp. 607-639.
- ↑ Lenci, Caduti dimenticati 1986, p. 234.
- ↑ Cox, Mary Elisabeth: Hunger in War and Peace. Women and Children in Germany, 1914-1924, Oxford 2019; Bessel, Germany After The First World War 1993, p. 40.
- ↑ Hamlin, David: Germany’s Empire in the East: Germans and Romania in an Era of Globalization and Total War, Cambridge 2017.
- ↑ Brendel, Heiko: “Lieber als Kacake als an Hunger sterben”. Besatzung und Widerstand im k.u.k Militärgeneralgouvernement in Montenegro (1916-1918), Frankfurt 2019.
- ↑ Özdemir, Hikmet: The Ottoman Army 1914-1918. Disease and Death on the Battlefield, Salt Lake City 2008, pp. 122-123.
- ↑ Gatrell, Peter: A Whole Empire Walking. Refugees in Russia during World War I, Bloomington 1999; Gatrell, Peter: The Making of the Modern Refugee, Oxford 2013, pp. 21-51.
- ↑ Gatrell, A Whole Empire Walking 1999, p.56.
- ↑ K. K. Ministerium des Innern: Staatliche Flüchtlingsfürsorge im Kriege 1914/15, Vienna 1915.
- ↑ Herrmann, Martina: “‘Cities of Barracks.’” Refugees in the Austrian part of the Habsburg Empire during the First World War,” in: Gatrell, Peter/Zhvanko, Liubov (eds.): Europe on the Move. Refugees in the Era of the Great War, Manchester 2017, p. 148; Judson, Pieter: The Habsburg Empire. A New History, Cambridge, MA 2016, pp. 408-415.
- ↑ Cases of dysentery-related deaths were reported between Austro-Hungarian and German POWs in Romanian camps; Archives of the International Committee of the Red Cross (ACICR), Camps en Roumanie, C G1 A 41-02.05, Geneva, Switzerland.
- ↑ Kramer, Alan: Prisoners in the First World War, in: Sibylle, Scheipers: Prisoners in War, Oxford 2010, pp. 78.
- ↑ Rasmussen, Anne: The Spanish Flu, in: Winter, Jay (ed.): The Cambridge History of the First World War, Volume III. Civil Society, Cambridge 2014, pp. 334-357.
- ↑ Oxford, J.S.: The so-called Great Spanish Influenza Pandemic of 1918 may have originated in France in 1916, in: The Royal Society (2001), pp. 1857-1859; Humphries, Mark Osborne: Paths of Infection: The First World War and the Origins of the 1918 Influenza Pandemic, in: War in History, 21/ 1 (2014), pp. 55-81.
- ↑ Gerwarth, Robert/Manela, Erez: The Great War as a Global War: Imperial Conflict and the Reconfiguration of World Order, 1911-1923, in: Diplomatic History, 38/4 (2014, pp. 786- 800.
- ↑ See Rice, Geoffrey/ Bryder, Linda: Black November: The 1918 Influenza Pandemic in New Zealand, Christchurch 2005; Rice, Geoffrey/Palmer, Edwina: Pandemic Influenza in Japan, 1918-19: Mortality patterns and Official Responses, in: The Journal of Japanese Studies, 19/2 (Summer 1993), pp. 389-420.
- ↑ “The Annual Report of the Sanitary Commissioner with the Government of India for 1919,” Indian Medical Gazette (October 1921), online: https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC5166378&blobtype=pdf (retrieved 3 November 2020); “Influenza in Bombay,” The Indian Medical Gazette (December 1918), accessed at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5136161/pdf/indmedgaz71832-0031.pdf (retrieved 2 November 2020).
- ↑ Phillips, Howard: Black October: the impact of the Spanish Influenza Epidemic of 1918 on South Africa, Pretoria 1990.
- ↑ Hersch, Liebmann: La mortalité causée par la guerre mondiale, in Metron. The International Review of Statistics, 7/1 (1927); Wilcox, Walter: Population and the World War. A Preliminary Survey, in: Journal of the American Statistical Association, 18/142 (1923), pp. 699-712; Huber, Michel: La population de la France pendant la guerre, Paris 1931.
- ↑ Mitchell, T.J / Smith, G.M.: Medical Services: Casualties and Medical Statistics of the Great War, London 1931, p.12.
- ↑ Winter, Jay: The Great War and the British People, London 2003, p. 123.
- ↑ Huber, La population de la France 1931, p. 282.
- ↑ Murard, Lion/ Zylberman, Patrick: The Nation Sacrificed for the Army? The Failing French Public Health, 1914-1918, in Eckart/Gradmann (eds.), Die Medizin und Der Erste Weltkrieg 2003, pp. 349-350.
- ↑ Gini, Corrado. I morti dell’esercito italiano dal 24 maggio 1915 al 31 dicembre 1918, Rome 1926.; Mortara, Giorgio: La salute pubblica in Italia durante e dopo la Guerra, New Haven 1925.
- ↑ Snowden, Frank: Naples in the Time of Cholera, 1884-1911, Cambridge 2002.
- ↑ Lenci, Giuliano: Caduti dimenticati. I moirti per malattie, in: Leoni, Diego/Zadra, Camillo (eds.): La Grande Guerra: Esperienza, Memoria, Immagini, Bologna 1986, pp. 234.
- ↑ Mortara, La salute pubblica in Italia, pp. 374-401.
- ↑ Heeres-Sanitätsinspektion des Reichswehrministeriums (ed.): Sanitätsbericht über das Deutsche Heer im Weltkriege 1914/18, Vol. 3, Die Krankenbewegung bei dem Deutschen Feld-und Besatzungsheer, Berlin 1934.
- ↑ Other diseases were dermatological diseases, disorders of internal organs, eye diseases or injury etc. See Whalen, Robert Weldon: Bitter Wounds, German Victims of the Great War, Ithaca 1984, pp. 52-53.
- ↑ Bessel, Richard: Germany After the First World War, Oxford 1993, p.39.
- ↑ Rumpler, Helmut/ Schmied-Kowarzik, Anatol (eds.): Weltkriegsstatistik Österreich-Ungarn 1914–1918. Bevölkerungsbewegung, Kriegstote, Kriegswirtschaft = Die Habsburgermonarchie 1848–1918 XI/2, Vienna 2014.
- ↑ Erickson, Edward J.: Ordered to Die: A History of the Ottoman Army in The First World War, Wesport/London 2001, p. 211.
- ↑ Özdemir, The Ottoman Army 2008, p. 131.
- ↑ Kohn, Stanislas/ Meynderoff, and Baron, Alexander: The Cost of the War to Russia, New Haven 1932.
- ↑ Bucur, Maria: Eugenics and Modernization in Interwar Romania, Pittsburgh 2010, p. 191.
- ↑ For an overview of historiography and analysis of data see Phillips, Howard: Influenza Pandemic , in: 1914-1918-online. International Encyclopedia of the First World War, ed. by Ute Daniel, Peter Gatrell, Oliver Janz, Heather Jones, Jennifer Keene, Alan Kramer, and Bill Nasson, issued by Freie Universität Berlin, Berlin 2014-10-08. DOI: 10.15463/ie1418.10148. (retrieved 2 November 2020).
- ↑ Murard/Zylberman, The Nation 2003.
- ↑ Van Bergen, Leo: Military Medicine, in: Winter, Jay (ed.): The Cambridge History of the First World War, Volume III. Civil Society, Cambridge 2014, p. 288;
- ↑ Herwig, The First World War 2014, p. 299.
- ↑ Tanielian, Melanie S.: The Charity of War. Famine, Humanitarian Aid, and World War I in the Middle East, Stanford 2018, pp. 141-170.
- ↑ Harrison, Medical War 2010, pp. 151-152.
- ↑ Linton, “War Dysentery”, pp. 607-639.
- ↑ Clarke, Nic/ Cranfield, John/ Inwood, Kris: Fighting Fit? Diet, Disease, and Disability in the Canadian Expeditionary Force, 1914-18, in: War & Society, 33/2 (May 2014), pp. 80-97.
- ↑ Soubbotitch, A Pandemic of Typhus, pp. 33-36.
- ↑ Rosenthal, Daniel: Confronting the Bacterial Enemy. Public Health, Philanthropy, and Jewish Responses to Typhus in Poland, 1914-1921, in: Rozenblit, Marsha L./Karp, Jonathan (eds.): World War I and the Jews: Conflict and Transformation in Europe, The Middle East, and America, New York 2017, pp. 131-150.
- ↑ Tanielian, The Charity of War 2018, pp. 141-170.
- ↑ Winter, Jay: The Impact of the First World War on Civilian Health in Britain” in: The Economic History Review, 30/3 (1977), pp. 487-507.
- ↑ Phillips, Influenza Pandemic.
- ↑ Faron, Olivier: Aux cotés, avec, pour les pupilles de la nations. Les forms de mobilization en faveur des orphelins de la Premiere Guerre Mondiale, in: Guerres Mondiales et Conflits Contemporains, 1/205 (2002), pp. 15-33.
- ↑ Weindling, Paul: The Medical Profession, Social Hygiene and the Birth Rate in Germany, 1914-18, in: Wall, Richard/Winter, Jay (eds): The Upheaval of War. Family, Work and Welfare in Europe, 1914-1918, Cambridge 1988, pp. 425.
- ↑ Rechter, David: Galicia in Vienna. Jewish Refugees in the First World War, in: Austrian History Yearbook Vol. 28 (1997), pp. 113-130.
- ↑ Kind-Kovacs, Friederike: The Great War, the child’s body and the American Red Cross, in: European Review of History: Revue europeene d’histoire, 23/1-2: Humanitarianisms in Context: Histories of Non-State Actors, From the Local to the Global (2016), pp. 33-62.
- ↑ Rosenthal, Confronting the Bacterial Enemy, pp. 134-135.
- ↑ Hetty Goldman Report, 29 April 1919, Folder Romania General 1919, Digital ID 230399, Collection New York Office 1919-1921, JDC Archives.
- ↑ Rozenblit, Marsha L: Reconstructing a National Identity. The Jews of Habsburg Austria during World War I, Oxford 2001.
- ↑ Cotter, Cedric: (S')Aider pour survivre. Action humanitaire et neutralité suisse pendant la Première Guerre Mondiale, Zurich 2018; Khan, Daniel-Erasmus: Das Rote Kreuz. Geschichte einer humanitären Weltbewegung, Munich 2013.
- ↑ Rachamimov, Alon: POWs and The Great War: Captivity on the Eastern Front, Oxford 2002, pp. 172-190.
- ↑ Makita, Yoshiya: The alchemy of humanitarianism: the First World War, the Japanese Red Cross and the creation of an international public health order, in: First World Wat Studies, 5/1 (2014), pp. 117-129.
- ↑ Irwin, Julia: Making the World Safe. The American Red Cross and a Nation’s Humanitarian Awakening, Oxford 2013.
- ↑ Stibbe, Matthew: The Internment of Civilians by Belligerent States during the First World War and the Response of the International Committee of the Red Cross, in: Journal of Contemporary History, 4/1 (2006), pp. 5-19; Jones, Heather: Violence against Prisoners of War in the First World War, Cambridge 2011, pp. 254-314.
- ↑ Gerwarth, Robert: The Vanquished. Why the First World War Failed to End, 1917-1923, London 2016; Newman, John Paul: The Origins, Attributes, and Legacies of Paramilitary Violence in the Balkans, in: Gerwarth, Robert/Horne, John (eds.): War in Peace. Paramilitary Violence in Europe after the Great War, Oxford 2012, pp. 145-163.
- ↑ Winter, The Impact of the First World War.
- ↑ Goodall, E.W: Typhus Fever in Poland, 1916 to 1919, in: Proceedings of the Royal Society of Medicine Vol.13 (1920), pp. 261-276.
- ↑ Durand, André: From Sarajevo to Hiroshima. History of the International Committee of the Red Cross, Geneva 1978, pp. 204-205.
- ↑ Irwin, Julia: “Sauvons les Bébés.” Child Health and US Humanitarian Aid in the First World War Era, in: Bulletin of the History of Medicine, 86/1 (2012), pp. 37-65; Rodogno, Davide: American Red Cross and the International Committee of the Red Cross’ humanitarian politics and policies in Asia Minor and Greece, in: First World War Studies, 5/1 (2014), pp. 83-99.
- ↑ Granick, Jaclyn: Humanitarian Responses to Jewish Suffering Abroad by American Jewish Organizations, 1914- 1929. PhD Thesis, The Graduate Institute of International and Development Studies, Geneva 2015, pp. 237-307.
- ↑ Dr. Clemens von Pirquet, 3 November 1921, Box 632, Folder 2, European Children’s Fund File, Register of the American Relief Administration European records, Reel 744, Microfilms Collection, Hoover Institution Archives, Stanford, CA, USA.
- ↑ Proctor, Tammy M.: An American enterprise? British Participation in US Food Relief Programmes (1914-1923), in: First World War Studies, 5/1 (2014), pp. 29-42.
- ↑ Weindling, Paul: Public Health and Political Stabilization: the Rockefeller Foundation in Central and Eastern Europe between the Two World Wars,” in: Minerva, 31/3, (Autumn 1993), pp. 253-267.
- ↑ Fischer, Marilyn: Caring Globally: Jane Addams, World War One, and International Hunger, in: Whisnant, Rebecca/DesAutels, Peggy (eds.): Global Feminist Ethics, New York 2008, pp.68-69.
- ↑ Borowy, Iris: Coming to Terms with World Health: The League of Nations Health Organisation 1921-1946, Frankfurt am Main 2009.
Selected Bibliography
- Borowy, Iris: Coming to terms with world health. The League of Nations health organisation 1921-1946, Frankfurt a. M. 2009: Lang.
- Cotter, Cédric: (S')aider pour survivre. Action humanitaire et neutralité suisse pendant la Première Guerre mondiale, Chêne-Bourg 2017: Georg Editeur.
- Cox, Mary Elizabeth: Hunger in war and peace. Women and children in Germany, 1914-1924, Oxford 2019: Oxford University Press.
- Eckart, Wolfgang Uwe / Gradmann, Christoph (eds.): Die Medizin und der Erste Weltkrieg, Pfaffenweiler 1996: Centaurus-Verlagsgesellschaft.
- Gatrell, Peter: A whole empire walking. Refugees in Russia during World War I, Bloomington 2011: Indiana University Press.
- Harrison, Mark: The medical war. British military medicine in the First World War, Oxford; New York 2010: Oxford University Press.
- Herwig, Holger H.: The First World War. Germany and Austria-Hungary, 1914-1918, London; New York 1997: Arnold; St. Martin's Press.
- Irwin, Julia: Making the world safe. The American Red Cross and a nation's humanitarian awakening, New York 2013: Oxford University Press.
- Jones, Heather: Violence against prisoners of war in the First World War. Britain, France, and Germany, 1914-1920, Cambridge; New York 2011: Cambridge University Press.
- Karge, Heike / Kind-Kovács, Friederike / Bernasconi, Sara (eds.): From the midwife's bag to the patient's file. Public health in eastern Europe, Budapest 2017: Central European University Press.
- Khan, Daniel Erasmus: Das Rote Kreuz. Geschichte einer humanitären Weltbewegung, Munich; Vienna 2013: C. H. Beck.
- Michl, Susanne: Im Dienste des 'Volkskörpers'. Deutsche und französische Ärzte im Ersten Weltkrieg, Göttingen 2007: Vandenhoeck & Ruprecht.
- Özdemir, Hikmet: The Ottoman army, 1914-1918. Disease and death on the battlefield, Salt Lake City 2008: University of Utah Press.
- Phillips, Howard: Black October. The impact of the Spanish Influenza epidemic of 1918 on South Africa, Pretoria 1990: Government Printer.
- Promitzer, Christian / Trubeta, Sevasti / Turda, Marius (eds.): Health, hygiene and eugenics in southeastern Europe to 1945, Budapest 2011: Central European University Press.
- Rice, Geoffrey / Bryder, Linda: Black November. The 1918 influenza pandemic in New Zealand, Christchurch 2005: Canterbury University Press.
- Rosenthal, Daniel: Confronting the bacterial enemy. Public health, philanthropy, and Jewish responses to typhus in Poland 1914-1921, in: Rozenblit, Marsha / Karp, Jonathan (eds.): World War I and the Jews. Conflict and transformation in Europe, the Middle East, and America, New York 2017: Berghahn, pp. 131-150.
- Schulze-Tanielian, Melanie: The charity of war. Famine, humanitarian aid and World War I in the Middle East, Stanford 2018: Stanford University Press.
- Weindling, Paul: Epidemics and genocide in eastern Europe 1890-1945, Oxford 2000: Oxford University Press.
- Winter, Jay: The Great War and the British people, London 1985: Palgrave Macmillan.