Introduction↑
While war is no stranger to mangled bodies, the First World War was unprecedented as it created a significant number of mutilated and disfigured men, many more than in previous conflicts. This article focuses particularly on the Western Front, a battleground established early in the war, where new forms of weaponry created new types of bodily injury.[1] The siege-style warfare of bombing and shelling on the Western Front meant that significant numbers of men were killed and others badly wounded on the periphery of a direct hit. New developments in weapons such as machine guns and grenades and more frightening and mysterious weaponry such as poison gas created an unprecedented range of mutilating and disfiguring wounds internally and externally.[2] These innovations in weapons and unspecific targeting circumvented the basic personal safety equipment provided to the fighting men, such as helmets and gas masks, and wreaked havoc on the body. No part of the soldier’s body was safe. Limbs were shattered by shrapnel and needed to be amputated to save patients’ lives. Gas blistered lungs and caused lifelong breathing difficulties and blindness. Gunshot wounds left random scars on bodies, a permanent reminder of war. The nature of trench warfare on the Western Front meant that faces were particularly vulnerable to gunshot wounds. Repairing faces presented a challenge to the medical profession and exposed a new type of visual horror.
Since Joanna Bourke’s seminal book Dismembering the Male was published in 1996, there has been a growing interest from historians in the historiography of the impact of war, and its permanent and devastating effects on the body.[3] Wounding is discussed in texts that focus on medical care in the conflict, such as Leo van Bergen’s 1999 book, Before My Helpless Sight.[4] Although van Bergen’s book focussed on wounding in all warring nations on the Western Front, much of the research which followed his book has centred on individual nations. The work which centres on mutilation and disfigurement concentrates on the ways that men with specific wounds were treated in hospitals and rehabilitation centres and, after their demobilisation, the ways in which they negotiated their identity, health, and perceptions of those around them. Ana Carden-Coyne and Jeffrey Reznick have concentrated on Britain; Sabine Kienitz, Heather Perry, and Wolfgang Eckart have examined Germany; Beth Linker has analysed disabled veterans in the United States.[5] There have been few comparative studies except for Deborah Cohen’s study on disabled ex-servicemen’s experiences in Britain and Germany, Marjorie Gehrhardt’s study of facial disfigurement in Britain, France, and Germany and Susanne Michl’s book comparing Germany and France.[6] Sophie Delaporte’s study on the facially disfigured in France is the most specific, as it concentrates on a particular type of wound in one nation.[7] As might be expected, analysis of mutilation and disfigurement has been confined to the largest nations: Britain, France, and Germany, and to a lesser extent the United States, with the exception of Pieter Verstraete and Christine van Everbroeck’s work on Belgian soldiers’ wounds.[8] There remains plenty of scope for historians in the future to analyse the impact of this specific type of wounding, treatment regimens, and reception in other nations.
Medical Specialities and Specialist Hospitals↑
While there are a number of arguments centring on whether or not war advanced medical practice, war certainly led to new techniques and technologies in the field of treating cases of mutilation and disfigurement.[9] Complex war wounds led to collaboration between different medical specialities to repair unprecedented bodily damage.
Two medical specialties in particular developed new techniques to treat the vast numbers of cases of mutilating and disfiguring wounds. The first was orthopaedics. It was already an established medical speciality before the war, but throughout the war techniques were advanced and new technologies developed. Amputation was the most common operation performed by orthopaedic surgeons during the war. Plastic surgery also developed further as a result of the significant number of injuries to the face and head. Specifically concentrating on the face, plastic surgeons painstakingly operated to recreate some semblance of a soldier’s pre-war appearance. Developments in military medicine served to alleviate advances in weapons that caused bodily damage.
Dedicated hospitals and institutions were established to treat these specific wounds. Often, the hurried efforts of surgeons at the front meant that amputee soldiers required further surgical procedures to repair and improve their amputation. Patients also needed time to recover from surgery. Following procedures, a prosthesis needed to be fitted and rehabilitative therapy commenced. In many cases, specialist limb fitters were placed in hospitals to ensure that the soldiers or sailor received the best fitting prosthesis. Specialist hospitals were established as those with amputation required specific types of treatment and rehabilitation was important in order to return amputees to the work force to assist the war effort.
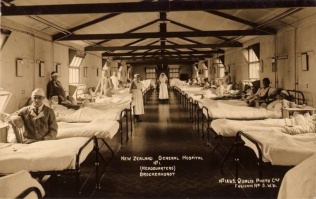
The organisation of hospitals and centres differed nationally. In Britain, the largest hospital for military amputees in England was Roehampton, a short distance outside London, and Erskine Hospital, just outside Glasgow, was the second largest.[10] The hospital facilities also housed limb-fitting workshops, where the amputee soldiers were fitted with their artificial limbs. There were significant numbers of specialist hospitals in Germany. At the hospitals, work therapy or Arbeitstherapie for amputees was the established method of rehabilitation, and a number of centres that focussed on different types of employment were set up for post-convalescence.[11] In most countries, hospitals combined medical care and rehabilitative regimes with the fitting of limbs and training for work. In the United States, two hospitals became centres for orthopaedic care – the Letterman General Hospital in San Francisco and the Walter Reed General Hospital in Washington.[12]
High quality centres for the treatment of facial wounds were established by a number of doctors during the war. In Britain, Harold Gillies (1882-1960) opened a specialist hospital, the Queens Hospital, to treat soldiers with facial wounds. The Dominions, Canada, New Zealand, and Australia provided specialist surgeons for their own soldiers at the hospital in the southeast of England, which by 1918 contained more than a thousand beds.[13] Gillies had originally worked with dentist, Charles Valadier (1873-1931), at the front and they concentrated on a combination of functional repair and the aesthetic of the face. In Paris, Hippolyte Morestin (1869-1919) worked to repair the faces of French soldiers wounded in war. Jacques Joseph (1865-1934) operated at the Charité in Berlin, where he performed plastic surgery on the facially wounded men of the German army. As well as providing specialist surgical treatment, the hospitals in warring nations provided specific kinds of associated therapy. For disfiguring wounds of the face, particular care had to be taken with mental health issues as well as physical restoration.
Amputation↑
Limb amputation was one of the most common practices during the war. Many thousands of limbs were amputated and lives were saved through its use. It is estimated in Germany that the number of amputations totalled 67,000 and 41,000 in Britain.[14] Many soldiers believed that they would rather die than be maimed, yet doctors at the fronts saved many thousands of soldiers through amputation.
Limbs were amputated for a number of reasons. They were often shredded as a result of shrapnel or explosions; machine guns shattered bones in arms or legs. Compound fracture, or one where the bone was shattered and projected through the skin, was a complex wound, and limbs were often amputated.[15] Often there was no bone left to join together, and the threat of complications such as infection meant that performing an amputation was safer for the patient. Environmental conditions increased the number of amputations and not all amputations were the result of traumatic injury. On the Western Front, amputations were conducted in cases of trench foot, caused by poor foot hygiene and immersion in trenches full of water. Furthermore, infection was often a complication in wounds. If gas gangrene affected an arm or leg, further amputations were conducted in order to save the soldier’s life.
Much of the work for orthopaedic surgeons on all sides of the conflict was centred on amputation. Orthopaedic surgeons conducted amputations for centuries, and innovations in anaesthetic, antiseptic use, and a range of surgical techniques improved patient outcomes during the war. Specific methods, care, and surveillance were employed to improve results and survival rates, and these were communicated to other surgeons by senior practitioners. In 1915 in Germany, Fritz Lange (1864-1952) a Munich orthopaedist published a field manual for army doctors. In Kriegs-Orthopädie (War Orthopaedics) he outlined methods to treat and transport patients with shattered limbs.[16] In Britain, Robert Jones (1857-1933), who became Director of Military Orthopaedics published Notes on Military Orthopaedics in 1917.[17] Publications such as these provided less experienced surgeons with guidance on practices and techniques to improve surgical and post-operative outcomes.
Long-held views on surgical treatment were challenged during the First World War. The range of damage to the body was often so extensive that different methods were employed to ensure the patient’s survival. Debridement, where flesh was removed, which was not employed in the early part of the war, was rediscovered and used effectively to prevent complications. The flap amputation, where a piece of skin covered the exposed amputation site, creating a padded area to make a healthy stump, was common in the 19th century and was effectively used during the war.
Surgeons at the front and in hospitals in their home country conducted thousands of amputations, from fingers to legs. Many soldiers endured multiple amputations, as the force of an explosion tore limbs from the body. However, American-born Ethelbert “Curley” Christian (1882-1954) who served in the Canadian army, was thought to be the only soldier to survive having all four of his limbs amputated.
Many surgeons became very skilled in the art of amputation through extensive practice. Surgeons at the front or on-board ships often amputated numbers of patients at a time. Often their hurried procedures left painful nerves exposed or an unsuitable stump so those amputations were tidied up away from the front by hospital surgeons who had more time to perform surgery in less pressured conditions. Some soldiers had four or five re-amputations in order to create a stump suitable for a prosthesis to be fitted.
There was much discussion amongst surgeons about where to amputate. In the First World War, surgeons undertook the practice of limb saving, which meant that they amputated as little of the limb as possible. One of the most important factors for a patient’s successful recovery after amputation was the correct surgical creation of the stump. Irregular stumps often made it difficult for technicians to fit an artificial limb. The stump was a vital component of the body-prosthesis nexus and needed to be surgically well-formed in order to provide a strong basis for the good fit and the best function of the prosthesis.
The stump had to be strong and painless. Many soldiers endured bulbar nerve surgery, as their stumps were sometimes painful due to exposed nerves. While they were in the hospital, many soldiers hardened their stumps by rubbing them with methylated spirits and wrapped them in tight bandages as they were healing. The stump also needed to shrink before it was fitted with a prosthesis. Soldiers learned to use their artificial limbs which often took many months. Early in the war, many soldiers were discharged from hospitals early, as hospitals experienced difficulty coping with the number of amputees. However, lack of instruction in the use of the limb affected soldiers’ stumps and, as one soldier noted, hospitals were full of men requiring treatment for sores on their stumps.[18]
Prosthetics↑
Prostheses were provided for amputee soldiers. New materials and designs were developed, ensuring that amputees were provided with the most advanced artificial limb available. Nations mobilised designers to create prosthetic limbs and a workforce to make them. In Germany, a great deal of effort was put into developing new devices to assist amputees.[19] Owing to their experience in the Civil War, American manufacturers, whose numbers had increased significantly after that conflict, were invited to Britain to share their expertise and develop new prosthetics.[20] For the first time, limb manufacturers worked closely with surgeons, a co-operation between the art of surgery and the craft of limb manufacture and fitting.
In the early part of the war, limb designs were similar to those developed in the 19th century. Heather Perry states that from the beginning of the war, German orthopaedists realised that they would need better prosthetics than were available.[21] Usually, arms and legs were made of wood, although metal was used as the war progressed, and were attached to the body using a range of leather straps and laces. A full leg amputation was often attached with a strap over the shoulder, as wooden prosthetic legs were very heavy. Arms were attached to the body with complicated harnesses, which often made them quite difficult to use.
As there were so many amputees, the pace of production of prosthetics was difficult to maintain throughout the war. One American orthopaedic surgeon estimated in 1915 that French limb makers were only able to manufacture 700 prostheses for the 7,000 amputees that required them.[22] In Britain, some of the 200 American prosthetic limb manufacturers were invited to establish workshops at the Queen Mary’s Limb fitting hospital at Roehampton, just outside London.[23] As many soldiers required prostheses, attempts to improve the speed at which limbs were supplied by making standard parts and fitting them together was adopted. Nevertheless, the number of amputees put pressure on the limb fitter’s ability to make the prosthesis and train the amputees to use their artificial limbs effectively. Limb fitters, surgeons, and disabled soldiers were concerned with three main issues: fit, function and camouflage.
Prosthetic arms were more difficult than legs to produce, as it was problematic to attach arms to the body. A complicated series of leather straps and laces was required, which made an artificial arm heavy and difficult for the wearer to manoeuvre. A range of implements to fit the arm prosthesis were developed, including eating utensils and tools. Small design adjustments made a difference in improving the prosthesis’ usefulness to the soldier. Often, this made the limb aesthetically different, creating an unfamiliar limb and an altered human form. Efforts were made to maintain recognisable physical standards, yet make limbs functional. The Openshaw hand had two little fingers strengthened with metal so that items could be carried. Yet functional limbs were not often very attractive to the public, so attempts were made to hide artificial limbs, particularly outside the work environment. In Germany, the “Sunday arm” was worn when a soldier wanted to disguise his amputation. If the limbs fitted well, functioned properly, and maintained standards of acceptable physiognomy, it was easier to hide the fact that a soldier or sailor wore an artificial limb.
Despite these new innovations, many artificial arms and legs were discarded when the men left hospital and only used on special occasions.[24] Poor fit, a lack of training in their use, and the soldier’s inability to adapt to the limb often meant that prostheses remained unused.
A prosthetic limb was compensation from the state for bodily loss, though some nations rewarded their disabled veterans more comprehensively than others. In addition to pensions, the British government provided a limb to each amputee veteran and by 1925 all amputees from the war were given a second limb as a substitute when a limb went for repair. In the United States, the Office of the Surgeon General effectively mandated the use of artificial limbs, to ensure that amputee veterans “passed” as able-bodied citizens after they were discharged.[25] In Germany, prostheses were provided by the state and centred on a veteran’s ability to work.
Mutilation↑
The bodies of the wounded were mutilated. Skin was cauterised and flayed from the body, burnt and mangled. Gunshot and shrapnel wounds left permanent marks and disfigurement. The skin on men’s trunks and backs was blistered and damaged from gas. Broken limbs could be repaired or removed and skin healed over what were once gaping wounds. But evidence of wounding left indelible marks on the body, which the medical profession could not remove. Moreover, the surgery required to repair injuries and sew skin together left visible scars. Amputation of a limb left a scarred stump. The mutilation of sexual organs was an issue that caused intense physical and psychological trauma, and for which nothing could be done. Wounds to soldiers’ sexual organs are rarely mentioned in the medical literature and there are few figures available on the number of soldiers who suffered this type of injury. In her book The Forbidden Zone, the former nurse Mary Borden (1886-1968) wrote about the level of damage to bodies including “mangled testicles”.[26] Not all disfigurement was external. Gas also caused internal wounds and scarring on the lungs, which caused breathing problems. The extent of the emotional impact of wounding was difficult to measure. The psychological and emotional trauma associated with disfigurement and mutilation went hand-in-hand with physical injury. There were many ways that war wounds affected the body and mind, causing permanent scarring.
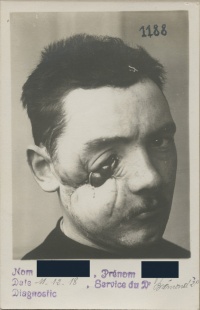
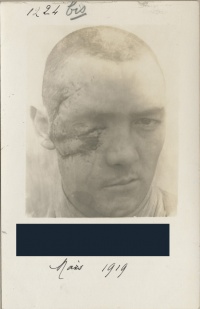
Evidence of disability caused through war wounds was often camouflaged. Bodily wounds were hidden by clothing, as with an arm or leg amputation. However, not all scarring could be disguised. One of the more common disfiguring wounds was to the face, and the effects of the damage was difficult to hide. Although surgical techniques developed extensively during the war, some faces were too badly mutilated and the only option was to hide the remaining mutilation. Masking the facially wounded was a way to integrate them into society. Prosthetic appliances for the face were developed before the First World War; in France, silver facial prostheses were developed as early as 1833.[27] During the First World War, new techniques were utilised for those whom surgery could not help. Artists were fundamental in the creation of camouflage of mutilated faces. In Britain, Frances Derwent-Wood (1871-1926) worked in what became known as the “tin noses shop” to create masks for British soldiers. In late 1917, after consultation with Wood, Anna Coleman-Ladd (1878-1939) opened the Studio for Portrait Masks in Paris, administered by the American Red Cross and situated in the city's Latin Quarter. In her workshop in France, Coleman-Ladd made masks for men to wear to hide their disfigured faces and became highly skilled at creating and fitting them.[28] Other artists such as Jane Poupelet (1874-1932) and Robert Wlérick (1882-1944) assisted Coleman-Ladd, and the studio was incorporated into the Vale-de-Grâce military hospital after the war.[29] Made of materials such as tin and enamel, the masks were carefully painted in the patient’s skin tones and correct eye colour to ensure a lifelike appearance. Ladd would take plaster casts of a soldier's face in an attempt to re-create an identical cheekbone or eye-socket on the opposite side. Ladd then crafted a full or partial mask out of copper, which she painted to match the skin while the soldier was wearing it. Of the nearly 3,000 or so French soldiers requiring masks, Ladd made about 185. These partial masks were attached to the face with spectacles or ribbon and provided the wearer the means to cover the parts of their faces that were missing or that contemporary surgical skill did not have the means to repair.
The masks were often uncomfortable to wear as the tin rubbed the face.[30] Many French veterans did not wear their masks, instead preferring to tie a cloth around the disfigured portion of their face.[31] The question remains: were the masks to protect the disfigured servicemen, or for the public who did not want to see the unsettling visage of the mutilated face? Some of the men rarely wore their masks, while other conceived it as an important part of their identity.
In national contexts, the experience of facial wounding differed radically. In Britain, many of those with facial wounds were isolated in hospitals. Conversely, in France, the gueules cassées named themselves as a distinct group of war wounded and established a powerful organisation which represented them.[32]
While many soldiers tried to hide the evidence of mutilation and the disfiguring impact of conflict on their bodies, the medical profession exposed the wounded and their wounds. Mutilation and disfigurement was documented through medical illustrations, paintings, and casts of wounds. Photography was used to chart a patient’s progress and demonstrate the healing process. Generally, these images and objects were used to train new medical personnel. Through this documentation, medical practitioners were able to track the progress of their outcomes and improve their practice. A number of artists, from sculptors to painters, documented the experience of wounded servicemen. In Germany, Joseph documented the healing of facial wounds of soldiers through photography. Albums full of photographs of the facially wounded from a hospital in Britain show their initial wound and the final result of many surgical procedures.[33] Other, more traditional forms of art were used to document soldiers and sailors’ wounds. In Britain, Henry Tonks (1862-1937) drew the facially wounded in pastel drawings for Gillies. Kathleen Scott (1878-1947), a noted sculptor, volunteered to help Gillies, declaring with characteristic aplomb that the "men without noses are very beautiful, like antique marbles." Artists from the British colonies and dominions also illustrated the wounding and recovery process, including New Zealander Herbert Cole (1867-1930) and Australian Daryl Lindsay (1889-1976).[34] In addition, the work of artists, photographers, and surgeons was designed to assist in the psychological healing process, which was just as important as the physical reconstruction of the face.
Plastic surgery↑
During the war, plastic surgery of the face became a medical specialty in itself. Surgical methods for repairing faces damaged as a result of gunshot wounds or shells advanced during the war. It has been argued that the sheer number of facially wounded men provided the means for surgeons to advance medical practice.[35] The number of injuries to the face was significant; it has been estimated that approximately 280,000 men suffered facial wounding in France, Germany, and Great Britain.[36]
Prior to the war, plastic surgery of the face was an established practice and certain areas of the face were surgically altered as related to social and cultural acceptability. In particular, surgeons operated and tried to surgically improve the aesthetics of syphilitic and “racially unacceptable” noses.[37] In cases of facial wounding, many surgeons merely sewed up wounds, less concerned with aesthetics than a successful surgical outcome. The smashed eye sockets, non-existent jaws, and noses presented by the war wounded were a real challenge to the technical expertise of surgeons. Repairing facial wounds became more an aesthetic exercise, as wounded servicemen got the best treatment possible for the sacrifice of their faces to the war effort. In some cases, the facially wounded soldier found it difficult to be accepted by his own family – let alone strangers whom he encountered. Instead of merely sewing up the face, the male aesthetic was considered in the surgical repair of the men’s faces. Indeed, Sander Gilman argues that the war had a positive effect on the acceptability of plastic surgery for aesthetic reasons.[38] He argues that reconstructive surgery became masculinised and therefore more acceptable. Yet plastic surgery in the First World War was more than just facial repair by a surgeon – it required a constant series of collaborations between surgeons, dentists, nurses, photographers, and artists. Reconstructive dentistry in particular was fundamental to the rebuilding of the face. The mechanical dentist provided knowledge of the reconstruction of the bones of the jaw, which provided the expertise and skill for the face to be rebuilt and functions such as chewing and swallowing restored. The collaboration between these individuals overlapped as expertise was required throughout the process of healing and reconstruction.[39]
This new approach and its collective of experts required spaces to treat patients. Surgeons persuaded their respective military medical authorities that they needed to set up special centres for treating maxillofacial wounds. Centres were established in all warring nations which provided specialist surgery, care, which helped men to accept and live with their disfigurement as well as they could outside the confines of the hospital. In Britain, facially wounded soldiers were sent to centres for treatment and were isolated from the wider public. Visits by the public to these hospitals were not encouraged as men grappled with accepting their frightening facial wounds. In these hospitals, mirrors were banned from the wards and benches in the local area were painted blue in order to warn the public that a soldier with facial wounds might sit there.[40]
Transporting soldiers with facial wounds to the hospitals was problematic. Often, for those with multiple wounds, the reconstruction of the face was left until last, as doctors dealt with other wounds considered life threatening. By the time patients got to specialist units, their faces had started to heal, which made reconstruction difficult for maxillofacial surgeons to repair their wounds.[41] In Britain, Harold Gillies went so far as to have tags printed with the address of his specialist unit at Aldershot hospital which were then distributed in field hospitals, so that he was able to conduct surgery and limit the permanent damage to the facially wounded soldier.[42]
Many surgeons and medical practitioners devised innovative ways to treat the facially wounded. One of the most successful innovations was the tubed pedicle. The procedure created a flap of skin from the chest or forehead, which was moved into place on the face.[43] The flap remained attached to the body, but was stitched into a tube to keep the blood supply intact and reduced the incidence of infection. Jaws were repaired by transplanting bone from other parts of the body, or using bones from other sources. While the results and outcomes were not always successful, a significant amount of effort was undertaken in order to restore the mutilated faces of soldiers.
Remembering the Disfigured and Mutilated↑
After the war, film, photography, and literature reminded the public of the physical effects of war on the body. In particular, the pacifist movement utilised depictions of mutilated men to highlight their anti-war message. The army of disabled men in all nations reminded the public of the human suffering that war caused. The impact of the war and its disfigured and mutilated had lasting cultural resonances, as seen throughout the century since its commencement, in the on-going production of a wide range of media relating to these men’s experiences and the war itself.
In different nations, the mutilated and disfigured from the war were treated differently. The veteran with an empty sleeve or trouser leg, an uneven gait, or a stiff arm with a gloved hand became commonplace in the post-war world. In many ways, their bodily loss represented their wartime experience, and was accepted by the public, often uneasy at the scale of the physical and emotional sacrifice of so many men. That said, many veterans with amputations walked carefully to hide their limp or wore a realistic hand or glove on their artificial arm in an attempt to disguise their amputation, no doubt for a number of reasons. However, those with facial disfigurement experienced complex feelings about their war service and their place in post-war society. The facially wounded in France, perhaps defiantly, showed their faces in public, whereas in other countries, many of those with facial disfigurements preferred to avoid exposure to a curious public. For many veterans mutilated and disfigured during the war, remembering their war service and devastating injuries was uncomfortable, and the physical reminder of the war – their missing body part, scarred body, weak lungs, or disfigured face – sometimes elicited unwanted attention.
The powerful and disturbing image of the disfigured and mutilated, particularly those with facial wounds, was used by a range of groups and individuals to convey a message. Pacifists used artists’ work to highlight the devastation of war, to ensure peace was maintained. The anti-war museum in Germany took photos of the mutilated and showed them in order to remind the public of the horrific maiming capacity of modern weaponry. Ernst Friedrich’s (1894-1967) War Against War showed twenty-four photographs from Joseph’s clinic at the Charité in Berlin to remind visitors to the exhibition of the terrifying visage that war created. Other artists such as Georg Grosz (1893-1959) who is probably best known for his work Ecce Homo (1922), also used the mutilated face to demonstrate the lasting horror of the legacy of war. After the war, exhibitions of casts of the disfigured faces of veterans were shown in hospitals in London, Berlin, and Paris.[44] It is difficult to ascertain the reasons why the public attended these exhibitions, but they served a potent reminder of the devastating effects of modern weaponry.
Novels, photography, and film have been inspired by the experiences of the war mutilated. The 2001 film La chambre des officiers, based on the novel by Marc Dugain, focused on the experiences of a number of officers in a specialist French facial ward. When a young boy is confronted by his father’s radically altered face, he shouts “Non mon papa, non mon papa!” The 1971 film Johnny’s Got His Gun was adapted from the 1938 novel of the same name written by Dalton Trumbo (1905-1976). Both films depicted the physical and mental trauma of the disfigured and mutilated from the war and reminded audiences that for some disabled veterans, the emotional trauma of war had to be overcome on a daily basis.
The prosthetics created by the association between medical personnel, crafts people, and artists are a physical reminder of the technology of war, as much as the weaponry which wrought the damage on the soldiers’ bodies and which fills war museums around the world. Some of the material culture of disfigurement in the First World War is ephemeral. Very few of the masks made so painstakingly by artists such as Derwent Wood and Coleman-Ladd exist. Some veterans came to depend heavily on their masks to camouflage their disfigurement, and as part of their physical construction of self, they were buried wearing them. Although numbers of facially wounded men did not wear their masks on a daily basis, special occasions warranted their use, similar to the German “Sunday arm”, which was saved for church to protect others’ sensibilities. Artificial limbs survive in greater numbers, probably because veterans had a number of them throughout their lives, and the prosthetic arms and legs were fashioned of wood, leather, and metal and possess a robustness that a thin tin mask does not.
The war mutilated and disfigured were remembered in public commemoration of the war, yet this differed in national contexts. Amputees were publicly remembered and participated in Armistice Day commemorations. Other veterans, whose clothes hid their disfigurement, also participated in the marches to various cenotaphs that took place around the world on the date selected for reflection on war and loss. However, the facially disfigured in many nations did not take part; instead they remained in the shadows of remembrance. In France, unlike many other nations, the public saw the mutilated as they paraded with other war wounded. National contexts are fundamental to understanding the treatment and life experience of the mutilated and disfigured from the war.
Conclusion↑
It is clear that the First World War produced many thousands of mutilated and disfigured men. Veterans with metal or wooden legs or empty sleeves were seen on the streets of large cities around the world for decades before the First World War and the 1914-1918 conflict added significant numbers of amputees. Those with facial mutilation, whose injuries were virtually impossible to disguise, added a new type of war horror, as the public saw their war-ravaged faces. Medical specialities were created and new spaces were established to treat the disfigured and mutilated. The war provided the means for new medical innovations to be developed in these institutions, and the number of wounded meant treatment and techniques were tested and proven during the war. Co-operation between medical professionals improved outcomes for the severely wounded. New therapeutic regimes and a state responsibility for treating the mutilated and disfigured meant that veterans from the war re-established themselves as useful working citizens. However, different forms of mutilation and disfigurement engendered different reactions from the veteran, those around them, and the state.
Julie Anderson, University of Kent
Section Editors: Michael Neiberg; Sophie De Schaepdrijver
Notes
- ↑ Significantly lowered death rates from disease as opposed to wounds were particular to the Western Front. For an overview of the impact of disease see Ozdemir, Hikmet: The Ottoman Army 1914-1918. Disease and Death on the Battlefield, Salt Lake City 2008.
- ↑ For details on weapons see Audoin-Rouzeau, Stephane: Weapons. Issued by 1914-1918 Online, online: http://encyclopedia.1914-1918-online.net/article/weapons.
- ↑ See Bourke, Joanna: Dismembering the Male. Men’s Bodies, Britain and the Great War. London 1996.
- ↑ See van Bergen, Leo: Before My Helpless Sight. Suffering, Dying and Military Medicine on the Western Front, 1914-1918, Farnham 2009.
- ↑ See Carden-Coyne, Ana: The Politics of Wounds. Military Patients and Medical power in the First World War, Oxford 2015; Reznick, Jeffrey S.: Healing the Nation. Soldiers and the Culture of Caregiving in Britain During the Great War, Manchester 2004; Reznick, Jeffrey S.: John Galsworthy and Disabled Soldiers of the Great War, Manchester 2009; Kienitz, Sabine: Beschädigte Helden. Kriegsinvalidität und Körperbilder 1914-1923, Paderborn 2008; Perry, Heather: Recycling the Disabled. Army, medicine and modernity in WW1 Germany, Manchester 2014; Eckart, Wolfgang U.: Medizin und Krieg. Deutschland 1914-1924, Paderborn 2014; Linker, Beth: War’s Waste, Rehabilitation in World War I America, Chicago 2011.
- ↑ Cohen, Deborah: The War Come Home. Disabled Veterans in Britain and Germany 1914-1939, Berkeley 2001; Gehrhardt, Marjorie: The Men with Broken Faces. Bern 2015; Michl, Susanne: Im Dienste des Volkskörpers. Deutsche und französische Ärzte im Ersten Weltkrieg, Göttingen 2007.
- ↑ Sophie, Delaporte: Les Gueules Cassées: Les Blessés de la Face de la Grande Guerre, Paris 1996.
- ↑ Verstraete, Pieter and Van Everbroeck, Christine: Le silence mutilé. les soldats invalides belges de la Grande Guerre, Namur (Belgium) 2014.
- ↑ See Cooter, Roger: Medicine and the Goodness of War, in: Canadian Bulletin of Medical History, 7/2 (1990).
- ↑ See Alper, Helen (ed.): A History of Queen Mary’s University Hospital Roehampton, Roehampton 1997. The University of Glasgow is currently cataloguing the Erskine House papers, online: https://universityofglasgowlibrary.wordpress.com/2016/03/29/launching-the-erskine-house-scheme/
- ↑ Perry, Recycling the Disabled 2014, p. 96.
- ↑ Linker, War’s Waste 2011, p. 81.
- ↑ Bamji, Andrew: Facial Surgery. the Patient’s Experience, in: Cecil, Hugh and Liddle, Peter H. (eds.): Facing Armageddon. The First World War Experienced, London 1996, p. 495.
- ↑ For Germany, see Whalen, Robert Gerald: Bitter Wounds. German Victims of the Great War, 1914-1939, Ithaca 1984, p. 40. For Britain, see Bourke, Dismembering the Male 1996.
- ↑ There were no sulphalidamides or antibiotics, which were not developed until the 1930s and the Second World War respectively.
- ↑ Perry, Recycling the Disabled 2014, p. 31.
- ↑ This was a collection of articles that had been published in medical journals such as the British Medical Journal.
- ↑ William Towers, 11038, Imperial War Museum Sound Archive, London.
- ↑ Anderson, Julie / Perry, Heather R.: Rehabilitation and Restoration. Orthopaedics and disabled soldiers in Germany and Britain in the First World War, in: Medicine, Conflict, and Survival, 30/4 (2014), p. 240.
- ↑ Conference on Artificial Limbs for Disabled Servicemen, in: British Medical Journal (31 July 1915), p. 190.
- ↑ Perry, Recycling the Disabled 2014, p. 46.
- ↑ Osgood, Robert B.: A Survey of the Orthopaedic Services in the US Army Hospitals, General Base and Debarkation, in: American Journal of Orthopaedic Surgery 17 (1919), pp. 359-82.
- ↑ Guyatt, Mary: Better Legs. Artificial Limbs for British Veterans of the First World War, in: Journal of Design History 14/4 (2001), p. 201.
- ↑ Heather, Perry: Re-arming the Disabled Veteran. Artificially Rebuilding State and Society in World War One Germany, in: Ott, Katherine et al. (eds.): Artificial Parts, Practical Lives. Modern Histories of Prosthetics, New York 2002.
- ↑ See Linker, War’s Waste 2011.
- ↑ Borden, Mary: The Forbidden Zone, London 2013, p. 43 [originally published in 1929].
- ↑ Wallace, Antony F.: The Progress of Plastic Surgery, Oxford 1982, p. 96.
- ↑ There is a short film of Anna Coleman-Ladd working in her studio in Paris with her assistants. The film depicts them making masks and fitting them to a disfigured soldier. Online: http://www.smithsonianmag.com/history/faces-of-war-145799854/.
- ↑ Gehrhardt, The Men with Broken Faces 2015, p. 49.
- ↑ Nicolson, Juliet: The Great Silence 1918-1920. Living in the Shadow of the Great War, London 2009, pp. 66-67.
- ↑ Delaporte, Sophie: Gueules Cassées de la Grande Guerre, in: Delaporte, F. / Fournier, E. / Devauchelle, B. (eds.): La Fabrique du Visage. De la Physiognomonie Antique à la Premiere Greffe du Visage, Turnhout 2010, p. 301.
- ↑ See Delaporte, Les Gueules Cassées 1996.
- ↑ Online: http://gilliesarchives.org.uk.
- ↑ Alberti, Samuel J.M.M. (ed.): War, Art and Surgery. The Work of Henry Tonks and Julia Midgley, London 2014, p. 9.
- ↑ Gehrhardt, The Men with Broken Faces 2015, p. 5.
- ↑ Winter, Jay: Forms of kinship and remembrance in the aftermath of the Great War, in: Winter, J. / Sivan, E. (eds.): War and Remembrance in the Twentieth Century, Cambridge 1999, p. 48.
- ↑ See Gilman, Sander L.: Making the Body Beautiful. A Cultural History of Aesthetic Surgery, Princeton 1999.
- ↑ Ibid., p. 164.
- ↑ Gerhardt argues that expertise was required in stages. Gehrhardt, The Men with Broken Faces 2015, p. 45.
- ↑ Bamji, Facial Surgery 1996, p. 498.
- ↑ Gehrhardt, The Men with Broken Faces 2015, p. 5.
- ↑ Bamji, Andrew: Queen Mary’s Sidcup, 1974-1994. A Commemoration, 1994, p. 13.
- ↑ Santoni-Rugiu, Paolo / Sykes, Philip J.: A History of Plastic Surgery, New York 2007, p. 96.
- ↑ Maliniak, Jacques W.: Sculpture in the Living. Rebuilding the Face and Form by Plastic Surgery, New York 1934, p. 30.
Selected Bibliography
- Alberti, Samuel J. M. M. (ed.): War, art and surgery. The work of Henry Tonks and Julia Midgley, London 2014: Royal College of Surgeons of England.
- Anderson, Julie: ‘Jumpy stump’. Amputation and trauma in the First World War, in: First World War Studies 6/1, 2015, pp. 9-19.
- Anderson, Julie / Perry, Heather R.: Rehabilitation and restoration. Orthopaedics and disabled soldiers in Germany and Britain in the First World War, in: Medicine, Conflict and Survival 30/4, 2014, pp. 227-251
- Biernoff, Suzannah: Flesh poems. Henry Tonks and the art of surgery, in: Visual Culture in Britain 11/1, 2010, pp. 25-47.
- Biernoff, Suzannah: The rhetoric of disfigurement in First World War Britain, in: Social History of Medicine 24/3, 2011, pp. 666-685.
- Bourke, Joanna: Dismembering the male. Men's bodies, Britain and the Great War, Chicago 1996: University of Chicago Press.
- Carden-Coyne, Ana: The politics of wounds. Military patients and medical power in the First World War, Oxford 2014: Oxford University Press.
- Carden-Coyne, Ana: Reconstructing the body. Classicism, modernism, and the First World War, Oxford 2009: Oxford University Press.
- Cohen, Deborah: The war come home. Disabled veterans in Britain and Germany, 1914-1939, Berkeley 2008: University of California Press.
- Delaporte, Sophie: Gueules cassées. Les blessés de la face de la Grande Guerre, Paris 2004: A. Viénot.
- Eckart, Wolfgang Uwe: Medizin und Krieg. Deutschland 1914-1924, Paderborn 2014: Ferdinand Schöningh.
- Gagen, Wendy Jane: Remastering the body, renegotiating gender. Physical disability and masculinity during the First World War, in: European Review of History. Revue europeenne d'histoire 14/4, 2007, pp. 525-541.
- Gehrhardt, Marjorie: The men with broken faces. Gueules cassées of the First World War, Oxford; Berlin 2015: Peter Lang.
- Harrison, Mark: The medical war. British military medicine in the First World War, Oxford; New York 2010: Oxford University Press.
- Kienitz, Sabine: Beschädigte Helden. Kriegsinvalidität und Körperbilder 1914-1923, Paderborn 2008: F. Schöningh.
- Linker, Beth: War's waste. Rehabilitation in World War I America, Chicago; London 2011: University of Chicago Press.
- Özdemir, Hikmet: The Ottoman army, 1914-1918. Disease and death on the battlefield, Salt Lake City 2008: University of Utah Press.
- Perry, Heather R.: Recycling the disabled. Army, medicine, and modernity in WWI Germany, Manchester 2014: Manchester University Press.
- Reznick, Jeffrey S.: John Galsworthy and disabled soldiers of the Great War. With an illustrated selection of his writings, Manchester 2009: Manchester University Press.
- Reznick, Jeffrey S.: Healing the nation. Soldiers and the culture of caregiving in Britain during the Great War, Manchester; New York 2004: Manchester University Press.
- Van Bergen, Leo: Before my helpless sight. Suffering, dying and military medicine on the Western Front, 1914-1918, Farnham; Burlington 2009: Ashgate.
- Weedon, Brenda, Alper, Helen (ed.): A history of Queen Mary's University Hospital Roehampton, Roehampton 1997: Richmond, Twickenham and Roehampton Healthcare NHS Trust.